Monday Poster Session
Category: IBD
P2568 - Systematic Review: Exploring the Potential of Metformin in Inflammatory Bowel Diseases
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AD
Aishwar Dixit, MBBS
Baba Raghav Das Medical College
Lucknow, Uttar Pradesh, India
Presenting Author(s)
Harshal Prakash Chorya, MBBS1, Sanjana Devaragudi, MBBS2, Aishwar Dixit, MBBS3, Kalyani Chowdary, MBBS4, Sweta Sahu, MBBS5
1Baroda Medical College, Vadodara, Gujarat, India; 2Apollo Institute of Medical Sciences and Research, Hyderabad, Telangana, India; 3Baba Raghav Das Medical College, Lucknow, Uttar Pradesh, India; 4Mahavir Institute of Medical Sciences, Vikarabad, Telangana, India; 5JJM Medical College, Devanagere, Karnataka, India
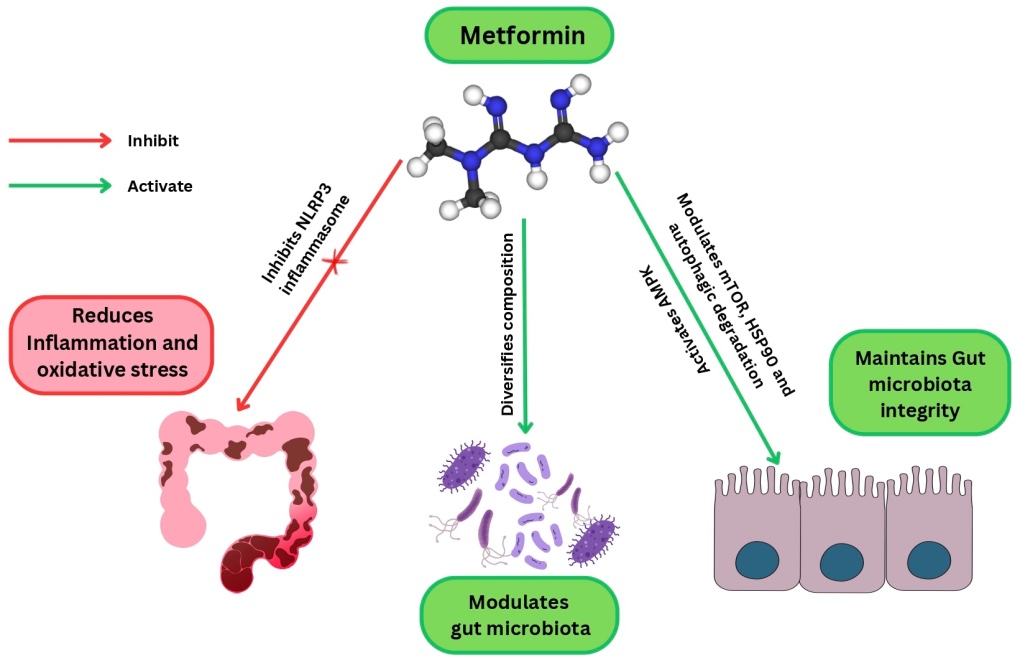
Introduction: This systematic review illuminates the multifaceted potential of metformin as a therapeutic intervention for Inflammatory Bowel Disease. Metformin’s anti-inflammatory effects are manifested through a variety of mechanisms, encompassing the inhibition of NF-κB activation, modulation of the AMPK pathway, adjustment of Th17/Treg balance, and suppression of pro-inflammatory cytokines. These multifaceted actions collectively contribute to its capacity to alleviate disease activity.
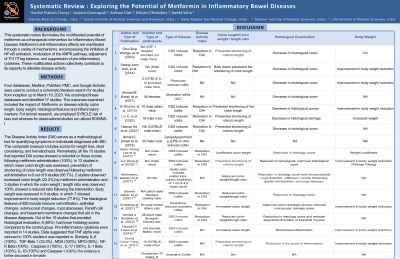
Methods: Four databases, Medline, PubMed, PMC, and Google Scholar, were used to conduct a schematic literature search for studies from inception up to March 19, 2023. We scrutinized these databases and identified 17 studies. We employed SYRCLE and ROBINS-I risk of bias tools. The outcomes examined included the impact of Metformin on disease activity, colon length, body weight, histological features and inflammatory markers.
Results: The Disease Activity Index (DAI) serves as a methodological tool for quantifying symptoms in individuals diagnosed with IBD. This composite measure includes scores for weight loss, stool consistency, and hematochezia. Remarkably, all the 10 studies that reported DAI scores showed a reduction in these scores following metformin administration (100%). In 12 studies in which mean colon length was assessed, prevention of shortening of colon length was observed following metformin administration in 6 out of 9 studies (66.7%). 2 studies observed increased colon length (22.2%) by metformin administration and 3 studies in which the colon weight / length ratio was observed, 100% showed a reduced ratio following the intervention. Body weight was assessed in 9 studies, in which 7 showed improvement in body weight reduction (77.8%). The histological features of IBD include immune cell infiltration, epithelial changes, submucosal changes, crypt abscesses, Paneth cell changes, and basement membrane changes that aid in the disease diagnosis. Out of the 15 studies that provided histological evaluation, 9 (60%) had lower histology scores compared to the control group. Pro-inflammatory cytokines were reported in 14 studies. Data suggested that TNF α was reduced in 100% studies it was reported in. Similarly, IL-6 (100%) , TGF-β 1 (33.3%) , MDA (100%), MPO (80%) , NF-Kβ(100%) , Caspase-3 (100%) , IL-17 (100%), IL-1 β (100%), IL-18 (100%) and Caspase-1 (100%).
Discussion: The evidence underscores Metformin’s anti-inflammatory properties through the various pathways and mechanisms in Table 1.0.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Harshal Prakash Chorya, MBBS1, Sanjana Devaragudi, MBBS2, Aishwar Dixit, MBBS3, Kalyani Chowdary, MBBS4, Sweta Sahu, MBBS5. P2568 - Systematic Review: Exploring the Potential of Metformin in Inflammatory Bowel Diseases, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Baroda Medical College, Vadodara, Gujarat, India; 2Apollo Institute of Medical Sciences and Research, Hyderabad, Telangana, India; 3Baba Raghav Das Medical College, Lucknow, Uttar Pradesh, India; 4Mahavir Institute of Medical Sciences, Vikarabad, Telangana, India; 5JJM Medical College, Devanagere, Karnataka, India
Introduction: This systematic review illuminates the multifaceted potential of metformin as a therapeutic intervention for Inflammatory Bowel Disease. Metformin’s anti-inflammatory effects are manifested through a variety of mechanisms, encompassing the inhibition of NF-κB activation, modulation of the AMPK pathway, adjustment of Th17/Treg balance, and suppression of pro-inflammatory cytokines. These multifaceted actions collectively contribute to its capacity to alleviate disease activity.
Methods: Four databases, Medline, PubMed, PMC, and Google Scholar, were used to conduct a schematic literature search for studies from inception up to March 19, 2023. We scrutinized these databases and identified 17 studies. We employed SYRCLE and ROBINS-I risk of bias tools. The outcomes examined included the impact of Metformin on disease activity, colon length, body weight, histological features and inflammatory markers.
Results: The Disease Activity Index (DAI) serves as a methodological tool for quantifying symptoms in individuals diagnosed with IBD. This composite measure includes scores for weight loss, stool consistency, and hematochezia. Remarkably, all the 10 studies that reported DAI scores showed a reduction in these scores following metformin administration (100%). In 12 studies in which mean colon length was assessed, prevention of shortening of colon length was observed following metformin administration in 6 out of 9 studies (66.7%). 2 studies observed increased colon length (22.2%) by metformin administration and 3 studies in which the colon weight / length ratio was observed, 100% showed a reduced ratio following the intervention. Body weight was assessed in 9 studies, in which 7 showed improvement in body weight reduction (77.8%). The histological features of IBD include immune cell infiltration, epithelial changes, submucosal changes, crypt abscesses, Paneth cell changes, and basement membrane changes that aid in the disease diagnosis. Out of the 15 studies that provided histological evaluation, 9 (60%) had lower histology scores compared to the control group. Pro-inflammatory cytokines were reported in 14 studies. Data suggested that TNF α was reduced in 100% studies it was reported in. Similarly, IL-6 (100%) , TGF-β 1 (33.3%) , MDA (100%), MPO (80%) , NF-Kβ(100%) , Caspase-3 (100%) , IL-17 (100%), IL-1 β (100%), IL-18 (100%) and Caspase-1 (100%).
Discussion: The evidence underscores Metformin’s anti-inflammatory properties through the various pathways and mechanisms in Table 1.0.
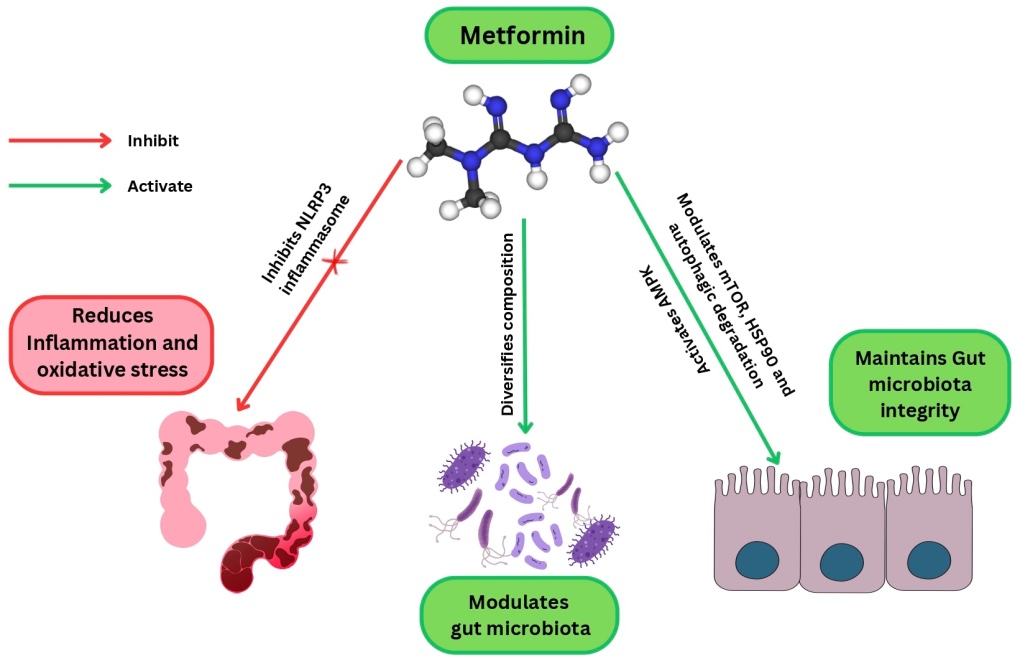
Figure: Potential of Metformin in Inflammatory Bowel Disease
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Harshal Prakash Chorya indicated no relevant financial relationships.
Sanjana Devaragudi indicated no relevant financial relationships.
Aishwar Dixit indicated no relevant financial relationships.
Kalyani Chowdary indicated no relevant financial relationships.
Sweta Sahu indicated no relevant financial relationships.
Harshal Prakash Chorya, MBBS1, Sanjana Devaragudi, MBBS2, Aishwar Dixit, MBBS3, Kalyani Chowdary, MBBS4, Sweta Sahu, MBBS5. P2568 - Systematic Review: Exploring the Potential of Metformin in Inflammatory Bowel Diseases, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
