Monday Poster Session
Category: IBD
P2595 - Bariatric Surgery Patients Have Lower Rates of Sepsis Compared to Non-Bariatric Patients When Hospitalized with Inflammatory Bowel Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Anusha Agarwal, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Roma Patel, MD1, Yazan Abu Omar, MD2, Stephen Firkins, MD3, Anusha Agarwal, MD4, C Roberto Simon-Linares, MD3
1Digestive Disease and Surgery Institute, Cleveland Clinic, Cleveland, OH; 2Digestive Disease Institute, Cleveland Clinic, Cleveland, OH; 3Cleveland Clinic, Cleveland, OH; 4Cleveland Clinic Foundation, Cleveland, OH
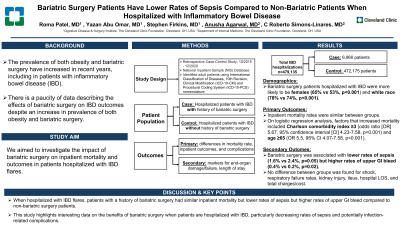
Introduction: There is a paucity of data describing the effects of bariatric surgery on IBD outcomes despite an increase in prevalence of both obesity and bariatric surgery. We aimed to investigate the impact of bariatric surgery on inpatient mortality and outcomes in patients hospitalized with IBD flares.
Methods: We performed a retrospective case-control study utilizing the National Inpatient Sample (NIS) database from 10/2015 to 12/2020. International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) and Procedural Coding System (ICD-10-PCS) nomenclature was used to identify all adults hospitalized with IBD (Crohn’s disease or ulcerative colitis) stratified into those with (case) and without (control) a history of bariatric surgery. Primary outcomes were differences in mortality rate and rates of inpatient outcomes and complications between patients with bariatric surgery and controls. Secondary outcomes were organ failures, including sepsis, shock, acute kidney injury (AKI) respiratory failure requiring mechanical ventilation as well as upper GI bleed and length of stay (LOS). Multivariate regression models were constructed to adjust for confounders and hospital characteristics.
Results: A total of 479,135 (weighted) IBD hospitalizations were included, 6,960 of which had history bariatric surgery. Bariatric surgery patients hospitalized with IBD were more likely to be females (65% vs 53%, p< 0.001) and white race (78% vs 74%, p< 0.001). Additionally, differences were found on the type of insurance, hospital size and region (Table 1). Inpatient mortality rates were similar among groups. Bariatric surgery was associated with lower rates of sepsis (1.6% vs 2.4%, p=0.05) but higher rates of upper GI bleed (0.4% vs 0.2%, p=0.02). On logistic regression analysis, factors that increased mortality included Charlson comorbidity index ≥3 (odds ratio [OR] 5.67, 95% confidence interval [CI] 4.23-7.58, p< 0.001) and age ≥65 (OR 5.5, 95% CI 4.07-7.58, p< 0.001).
Discussion: When hospitalized with IBD flares, patients with a history of bariatric surgery had similar inpatient mortality but lower rates of sepsis but higher rates of upper GI bleed compared to non-bariatric surgery patients. This study highlights interesting data on the benefits of bariatric surgery when patients are hospitalized with IBD, particularly decreasing rates of sepsis and potentially infection-related complications.
Disclosures:
Roma Patel, MD1, Yazan Abu Omar, MD2, Stephen Firkins, MD3, Anusha Agarwal, MD4, C Roberto Simon-Linares, MD3. P2595 - Bariatric Surgery Patients Have Lower Rates of Sepsis Compared to Non-Bariatric Patients When Hospitalized with Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Digestive Disease and Surgery Institute, Cleveland Clinic, Cleveland, OH; 2Digestive Disease Institute, Cleveland Clinic, Cleveland, OH; 3Cleveland Clinic, Cleveland, OH; 4Cleveland Clinic Foundation, Cleveland, OH
Introduction: There is a paucity of data describing the effects of bariatric surgery on IBD outcomes despite an increase in prevalence of both obesity and bariatric surgery. We aimed to investigate the impact of bariatric surgery on inpatient mortality and outcomes in patients hospitalized with IBD flares.
Methods: We performed a retrospective case-control study utilizing the National Inpatient Sample (NIS) database from 10/2015 to 12/2020. International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) and Procedural Coding System (ICD-10-PCS) nomenclature was used to identify all adults hospitalized with IBD (Crohn’s disease or ulcerative colitis) stratified into those with (case) and without (control) a history of bariatric surgery. Primary outcomes were differences in mortality rate and rates of inpatient outcomes and complications between patients with bariatric surgery and controls. Secondary outcomes were organ failures, including sepsis, shock, acute kidney injury (AKI) respiratory failure requiring mechanical ventilation as well as upper GI bleed and length of stay (LOS). Multivariate regression models were constructed to adjust for confounders and hospital characteristics.
Results: A total of 479,135 (weighted) IBD hospitalizations were included, 6,960 of which had history bariatric surgery. Bariatric surgery patients hospitalized with IBD were more likely to be females (65% vs 53%, p< 0.001) and white race (78% vs 74%, p< 0.001). Additionally, differences were found on the type of insurance, hospital size and region (Table 1). Inpatient mortality rates were similar among groups. Bariatric surgery was associated with lower rates of sepsis (1.6% vs 2.4%, p=0.05) but higher rates of upper GI bleed (0.4% vs 0.2%, p=0.02). On logistic regression analysis, factors that increased mortality included Charlson comorbidity index ≥3 (odds ratio [OR] 5.67, 95% confidence interval [CI] 4.23-7.58, p< 0.001) and age ≥65 (OR 5.5, 95% CI 4.07-7.58, p< 0.001).
Discussion: When hospitalized with IBD flares, patients with a history of bariatric surgery had similar inpatient mortality but lower rates of sepsis but higher rates of upper GI bleed compared to non-bariatric surgery patients. This study highlights interesting data on the benefits of bariatric surgery when patients are hospitalized with IBD, particularly decreasing rates of sepsis and potentially infection-related complications.
Disclosures:
Roma Patel indicated no relevant financial relationships.
Yazan Abu Omar indicated no relevant financial relationships.
Stephen Firkins indicated no relevant financial relationships.
Anusha Agarwal indicated no relevant financial relationships.
C Roberto Simon-Linares indicated no relevant financial relationships.
Roma Patel, MD1, Yazan Abu Omar, MD2, Stephen Firkins, MD3, Anusha Agarwal, MD4, C Roberto Simon-Linares, MD3. P2595 - Bariatric Surgery Patients Have Lower Rates of Sepsis Compared to Non-Bariatric Patients When Hospitalized with Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
