Monday Poster Session
Category: IBD
P2603 - Risk of Gynecologic Malignancies in Females With Crohn’s Disease: A Multi-Network Study
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Shaina Ailawadi, MD
University Hospitals Cleveland Medical Center, Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Shaina Ailawadi, MD1, Abdullah Mahmood, MD1, Elleson G. Harper, BS1, Jaime A. Perez, PhD2, Preetika Sinh, MD3, Gregory Cooper, MD4, Vu Q. Nguyen, MD, MS4, Jeffry Katz, MD4, Fabio Cominelli, MD, PhD4, Miguel D Regueiro, MD5, Emad Mansoor, MD4
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2University Hospitals Clinical Research Center, Cleveland, OH; 3Medical College of Wisconsin, Milwaukee, WI; 4Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 5Cleveland Clinic, Cleveland, OH
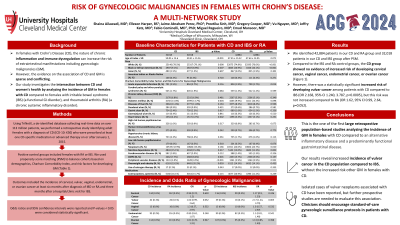
Introduction: In females with Crohn’s Disease (CD), the nature of chronic inflammation and immune dysregulation can increase the risk of extraintestinal manifestations including gynecologic malignancies (GM). However, the evidence on the association of CD and GM is sparse and conflicting. Our study investigates the intersection between CD and women’s health by analyzing the incidence of GM in females with CD compared to irritable bowel syndrome (IBS) (a functional GI disorder), and rheumatoid arthritis (RA) (a chronic systemic inflammatory disorder).
Methods: Using TriNetX, a de-identified database of over 113 million patients, we performed a retrospective study identifying adult females with a diagnosis of CD (ICD-10: K50) who were prescribed at least one CD-specific medication or advanced therapy on or after January 1, 2015. Positive control groups included females with RA or IBS. We used propensity score matching (PSM) to balance cohorts based on demographics, Charlson Comorbidity Index, and risk factors for developing GM (Table 1). Outcomes included the incidence of cervical, vulvar, vaginal, endometrial, or ovarian cancer at least six months after diagnosis of IBD or RA and three months after a hospital/clinic visit for IBS. Odds ratios and 95% confidence intervals were reported and P-values < 0.05 were considered statistically significant.
Results: We identified 42,884 patients in our CD and RA group and 32,018 patients in our CD and IBS group after PSM. Compared to the IBS and RA control groups, the CD group showed no evidence of increased risk of developing cervical cancer, vaginal cancer, endometrial cancer, or ovarian cancer. However, there was a statistically significant increased risk of developing vulvar cancer among patients with CD compared to IBS (OR 2.168, 95% CI 1.240, 3.787, p=0.0005), but this risk was not increased compared to RA (OR 1.62, 95% CI 0.99, 2.64, p=0.052).
Discussion: This is the one of the first large retrospective population-based studies analyzing the incidence of GM in females with CD compared to an alternative inflammatory disease and a predominantly functional gastrointestinal disease. Our results show increased incidence of vulvar cancer in the CD population compared to IBS, without the increased risk of other GM. Isolated cases of vulvar neoplasms associated with CD have been reported, but further prospective studies are needed to evaluate this. Clinicians should encourage standard-of-care gynecologic surveillance protocols in patients with CD.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Shaina Ailawadi, MD1, Abdullah Mahmood, MD1, Elleson G. Harper, BS1, Jaime A. Perez, PhD2, Preetika Sinh, MD3, Gregory Cooper, MD4, Vu Q. Nguyen, MD, MS4, Jeffry Katz, MD4, Fabio Cominelli, MD, PhD4, Miguel D Regueiro, MD5, Emad Mansoor, MD4. P2603 - Risk of Gynecologic Malignancies in Females With Crohn’s Disease: A Multi-Network Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2University Hospitals Clinical Research Center, Cleveland, OH; 3Medical College of Wisconsin, Milwaukee, WI; 4Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 5Cleveland Clinic, Cleveland, OH
Introduction: In females with Crohn’s Disease (CD), the nature of chronic inflammation and immune dysregulation can increase the risk of extraintestinal manifestations including gynecologic malignancies (GM). However, the evidence on the association of CD and GM is sparse and conflicting. Our study investigates the intersection between CD and women’s health by analyzing the incidence of GM in females with CD compared to irritable bowel syndrome (IBS) (a functional GI disorder), and rheumatoid arthritis (RA) (a chronic systemic inflammatory disorder).
Methods: Using TriNetX, a de-identified database of over 113 million patients, we performed a retrospective study identifying adult females with a diagnosis of CD (ICD-10: K50) who were prescribed at least one CD-specific medication or advanced therapy on or after January 1, 2015. Positive control groups included females with RA or IBS. We used propensity score matching (PSM) to balance cohorts based on demographics, Charlson Comorbidity Index, and risk factors for developing GM (Table 1). Outcomes included the incidence of cervical, vulvar, vaginal, endometrial, or ovarian cancer at least six months after diagnosis of IBD or RA and three months after a hospital/clinic visit for IBS. Odds ratios and 95% confidence intervals were reported and P-values < 0.05 were considered statistically significant.
Results: We identified 42,884 patients in our CD and RA group and 32,018 patients in our CD and IBS group after PSM. Compared to the IBS and RA control groups, the CD group showed no evidence of increased risk of developing cervical cancer, vaginal cancer, endometrial cancer, or ovarian cancer. However, there was a statistically significant increased risk of developing vulvar cancer among patients with CD compared to IBS (OR 2.168, 95% CI 1.240, 3.787, p=0.0005), but this risk was not increased compared to RA (OR 1.62, 95% CI 0.99, 2.64, p=0.052).
Discussion: This is the one of the first large retrospective population-based studies analyzing the incidence of GM in females with CD compared to an alternative inflammatory disease and a predominantly functional gastrointestinal disease. Our results show increased incidence of vulvar cancer in the CD population compared to IBS, without the increased risk of other GM. Isolated cases of vulvar neoplasms associated with CD have been reported, but further prospective studies are needed to evaluate this. Clinicians should encourage standard-of-care gynecologic surveillance protocols in patients with CD.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Shaina Ailawadi indicated no relevant financial relationships.
Abdullah Mahmood indicated no relevant financial relationships.
Elleson Harper indicated no relevant financial relationships.
Jaime Perez indicated no relevant financial relationships.
Preetika Sinh: Bristol Myers Squibb – Advisory Committee/Board Member.
Gregory Cooper indicated no relevant financial relationships.
Vu Nguyen: AbbVie – Speakers Bureau. Eli Lilly – Speakers Bureau.
Jeffry Katz indicated no relevant financial relationships.
Fabio Cominelli indicated no relevant financial relationships.
Miguel D Regueiro: AbbVie – Advisory Committee/Board Member, Consultant, Speakers Bureau.
Emad Mansoor: Lilly – Speakers Bureau. Takeda – Speakers Bureau.
Shaina Ailawadi, MD1, Abdullah Mahmood, MD1, Elleson G. Harper, BS1, Jaime A. Perez, PhD2, Preetika Sinh, MD3, Gregory Cooper, MD4, Vu Q. Nguyen, MD, MS4, Jeffry Katz, MD4, Fabio Cominelli, MD, PhD4, Miguel D Regueiro, MD5, Emad Mansoor, MD4. P2603 - Risk of Gynecologic Malignancies in Females With Crohn’s Disease: A Multi-Network Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
