Monday Poster Session
Category: IBD
P2634 - Comparing the Accuracy of Computed Tomography Enterography to Balloon-Assisted Enteroscopy in the Evaluation of Small Bowel Crohn’s Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
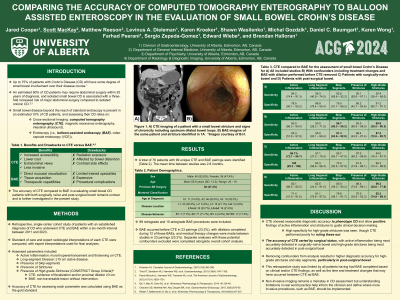
Has Audio

Scott MacKay, MD
University of Alberta
Edmonton, AB, Canada
Presenting Author(s)
Jared Cooper, MD, Scott MacKay, MD, Matthew Reeson, PhD, Levinus Dieleman, MD, PhD, Karen Kroeker, MD, MSc, Shawn Wasilenko, MD, PhD, Michal Gozdzik, MD, Daniel Baumgart, MD, PhD, MBA, Frank Hoentjen, MD, PhD, Karen Wong, MD, Farhad Peerani, MD, Sergio Zepeda-Gomez, MD, Edward Wiebe, MD, Brendan Halloran, MD
University of Alberta, Edmonton, AB, Canada
Introduction: Evaluation of small bowel Crohn’s Disease (CD) beyond the reach of standard endoscopy often relies on cross-sectional imaging such as computed tomography enterography (CTE) and small bowel endoscopy. Balloon-assisted enteroscopy (BAE) is frequently utilized in this clinical setting as it allows for mucosal visualization, tissue acquisition, and therapeutic capabilities. The accuracy of CTE in evaluating features of small bowel CD in both naïve and post-surgical bowel remains unclear compared to BAE.
Methods: Patients with an established diagnosis of small bowel CD who underwent a CTE and BAE within a six-month period between 2011 and 2023 were reviewed. Findings of active inflammation, long-segment disease, skip-segments, strictures, and presence of high-grade strictures (HGS) were extracted from both CTE and BAE studies and analyzed using BAE as the gold standard. Standard of care and expert interpretations by a radiologist with expertise in small bowel imaging were compared, with expert interpretations used for final analyses.
Results: A total of 76 patients with 99 corresponding unique CTE and BAE pairings were identified. CTE was most sensitive for active inflammation (84.2% (74.4 – 91.3) and strictures (92.1% (83.6 - 97.1)) and most specific for long segment inflammation (88.9% (78.4 – 95.4)) and HGS (91.2% (80.7 - 97.1)). CTE had low sensitivity for HGS (52.5%) and long segment inflammation (58.3%), and low specificity for strictures (65.2%). NPV was low overall for active inflammation (50.0%). In subgroup analyses, CTE demonstrated improved detection of active inflammation (sensitivity: 86.1%, specificity: 100%) in naïve bowel and, in post-surgical bowel, sensitivity for HGS improved modestly to 59.3% with a high specificity of 92.3%.
Discussion: CTE demonstrated reasonable accuracy for the use of positive identification of active inflammation and fibrostenotic lesions to guide clinical decision-making, but may be insufficient to rule out active inflammation and reliably detect HGS. The accuracy of CTE for detecting small bowel CD features differed between naïve and post-surgical bowel. Overall, CTE remains complementary to BAE in the assessment and management of small bowel CD.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jared Cooper, MD, Scott MacKay, MD, Matthew Reeson, PhD, Levinus Dieleman, MD, PhD, Karen Kroeker, MD, MSc, Shawn Wasilenko, MD, PhD, Michal Gozdzik, MD, Daniel Baumgart, MD, PhD, MBA, Frank Hoentjen, MD, PhD, Karen Wong, MD, Farhad Peerani, MD, Sergio Zepeda-Gomez, MD, Edward Wiebe, MD, Brendan Halloran, MD. P2634 - Comparing the Accuracy of Computed Tomography Enterography to Balloon-Assisted Enteroscopy in the Evaluation of Small Bowel Crohn’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Alberta, Edmonton, AB, Canada
Introduction: Evaluation of small bowel Crohn’s Disease (CD) beyond the reach of standard endoscopy often relies on cross-sectional imaging such as computed tomography enterography (CTE) and small bowel endoscopy. Balloon-assisted enteroscopy (BAE) is frequently utilized in this clinical setting as it allows for mucosal visualization, tissue acquisition, and therapeutic capabilities. The accuracy of CTE in evaluating features of small bowel CD in both naïve and post-surgical bowel remains unclear compared to BAE.
Methods: Patients with an established diagnosis of small bowel CD who underwent a CTE and BAE within a six-month period between 2011 and 2023 were reviewed. Findings of active inflammation, long-segment disease, skip-segments, strictures, and presence of high-grade strictures (HGS) were extracted from both CTE and BAE studies and analyzed using BAE as the gold standard. Standard of care and expert interpretations by a radiologist with expertise in small bowel imaging were compared, with expert interpretations used for final analyses.
Results: A total of 76 patients with 99 corresponding unique CTE and BAE pairings were identified. CTE was most sensitive for active inflammation (84.2% (74.4 – 91.3) and strictures (92.1% (83.6 - 97.1)) and most specific for long segment inflammation (88.9% (78.4 – 95.4)) and HGS (91.2% (80.7 - 97.1)). CTE had low sensitivity for HGS (52.5%) and long segment inflammation (58.3%), and low specificity for strictures (65.2%). NPV was low overall for active inflammation (50.0%). In subgroup analyses, CTE demonstrated improved detection of active inflammation (sensitivity: 86.1%, specificity: 100%) in naïve bowel and, in post-surgical bowel, sensitivity for HGS improved modestly to 59.3% with a high specificity of 92.3%.
Discussion: CTE demonstrated reasonable accuracy for the use of positive identification of active inflammation and fibrostenotic lesions to guide clinical decision-making, but may be insufficient to rule out active inflammation and reliably detect HGS. The accuracy of CTE for detecting small bowel CD features differed between naïve and post-surgical bowel. Overall, CTE remains complementary to BAE in the assessment and management of small bowel CD.
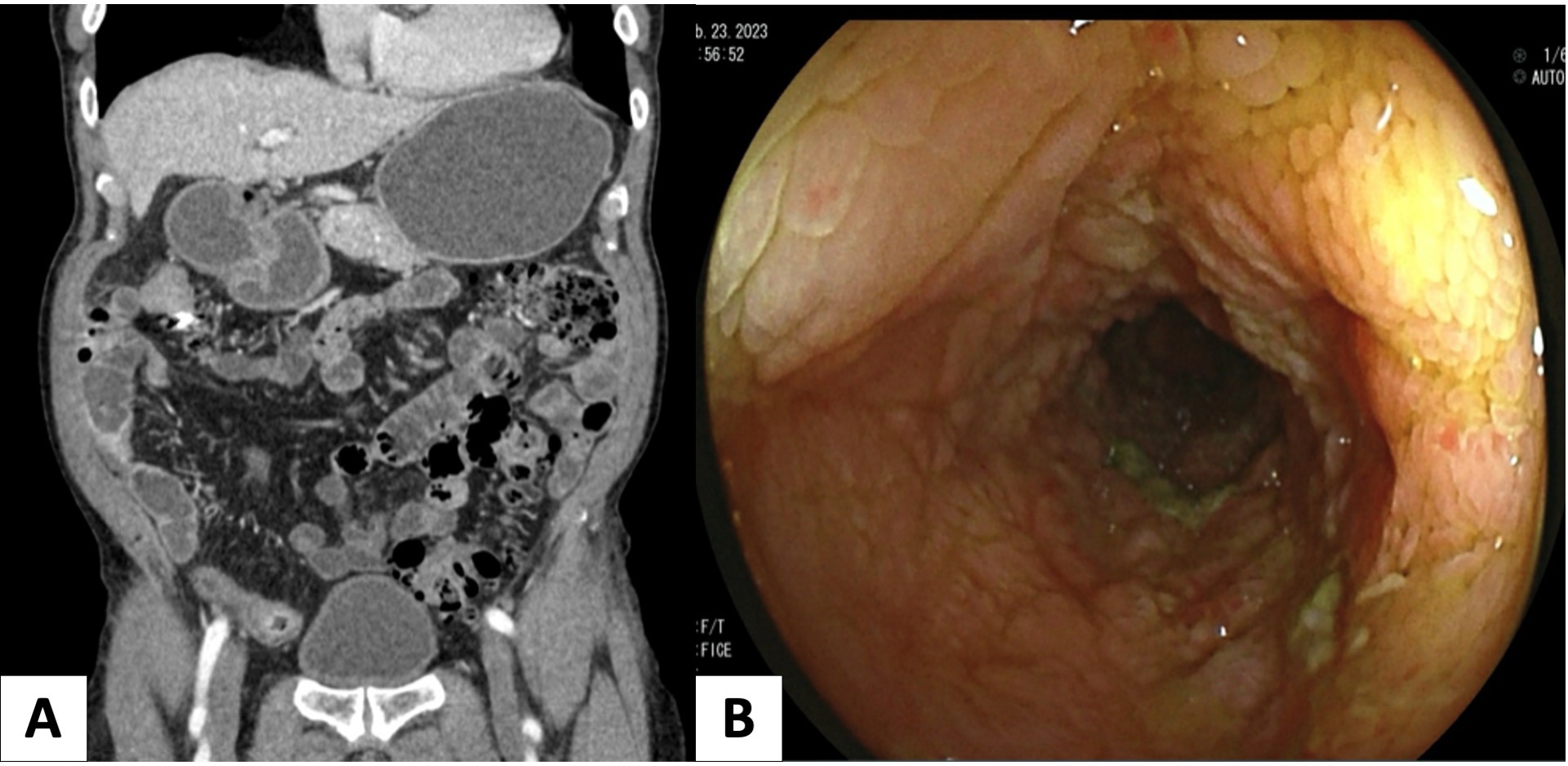
Figure: Figure 1. A) Computed Tomography Enterography (CTE) imaging of a patient with a small bowel stricture and signs of chronicity including upstream dilated bowel loops. B) Intra-procedure image of the same stricture identified in 1A taken during balloon-assisted enteroscopy (BAE).
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jared Cooper indicated no relevant financial relationships.
Scott MacKay indicated no relevant financial relationships.
Matthew Reeson indicated no relevant financial relationships.
Levinus Dieleman: Abbvie – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member.
Karen Kroeker: Abbvie – Advisory Committee/Board Member. Celltrion – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member. Pfizer – Speakers Bureau. Takeda – Advisory Committee/Board Member.
Shawn Wasilenko: Pentax – Advisory Committee/Board Member.
Michal Gozdzik: Pfizer – Grant/Research Support.
Daniel Baumgart: Abbvie – Advisory Committee/Board Member, Grant/Research Support. BMS – Advisory Committee/Board Member, Grant/Research Support. Janssen – Advisory Committee/Board Member, Grant/Research Support. Pfizer – Advisory Committee/Board Member, Grant/Research Support. Takeda – Advisory Committee/Board Member, Grant/Research Support.
Frank Hoentjen: Abbvie – Advisory Committee/Board Member, Grant/Research Support. Amgen – Advisory Committee/Board Member. Celltrion – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member, Grant/Research Support. Pendopharm – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member, Grant/Research Support. Takeda – Advisory Committee/Board Member.
Karen Wong: Abbvie – Speakers Bureau. Janssen – Advisory Committee/Board Member, Speakers Bureau.
Farhad Peerani: Abbvie – Advisory Committee/Board Member. BioJAMP – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member. Takeda – Advisory Committee/Board Member.
Sergio Zepeda-Gomez indicated no relevant financial relationships.
Edward Wiebe indicated no relevant financial relationships.
Brendan Halloran: Abbvie – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Celltrion – Advisory Committee/Board Member, Speakers Bureau. Ferring – Advisory Committee/Board Member, Speakers Bureau. Fujifilm – Speakers Bureau. Innomar – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Pendopharm – Speakers Bureau. Pfizer – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Shire – Speakers Bureau. Takeda – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau.
Jared Cooper, MD, Scott MacKay, MD, Matthew Reeson, PhD, Levinus Dieleman, MD, PhD, Karen Kroeker, MD, MSc, Shawn Wasilenko, MD, PhD, Michal Gozdzik, MD, Daniel Baumgart, MD, PhD, MBA, Frank Hoentjen, MD, PhD, Karen Wong, MD, Farhad Peerani, MD, Sergio Zepeda-Gomez, MD, Edward Wiebe, MD, Brendan Halloran, MD. P2634 - Comparing the Accuracy of Computed Tomography Enterography to Balloon-Assisted Enteroscopy in the Evaluation of Small Bowel Crohn’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
