Monday Poster Session
Category: IBD
P2661 - Endoscopic Showdown: Balloon Dilation vs Stricturotomy vs Stenting for Inflammatory Bowel Disease Strictures - A Systematic Review and Meta-Analysis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Partha Pal, MD
Asian Institute of Gastroenterology
Hyderabad, Telangana, India
Presenting Author(s)
Partha Pal, MD1, Rajesh Gupta, MD, DM1, Manu Tandan, MD, DM1, D Nageshwar Reddy, MD, DM, FACG1, Gursimran S. Kochhar, MD2
1Asian Institute of Gastroenterology, Hyderabad, Telangana, India; 2Allegheny General Hospital, Pittsburgh, PA
Introduction: Resection for inflammatory bowel disease (IBD) strictures carries risks of morbidity, recurrence, and short bowel syndrome. Endoscopic therapies like balloon dilation (EBD), stenting, and stricturotomy (ES) offer alternative treatments with varying success, re-intervention needs, and adverse effects. However, prospective comparative studies on these techniques are lacking, necessitating further research to guide clinical practice.
Methods: A literature search was conducted using PubMed and Embase, spanning 1985 to May 2024. This meta-analysis focused on primary outcomes—clinical success and secondary outcomes including technical succes, adverse events, re-intervention, and need for surgery. Analyses were performed using MedCalc,v22.
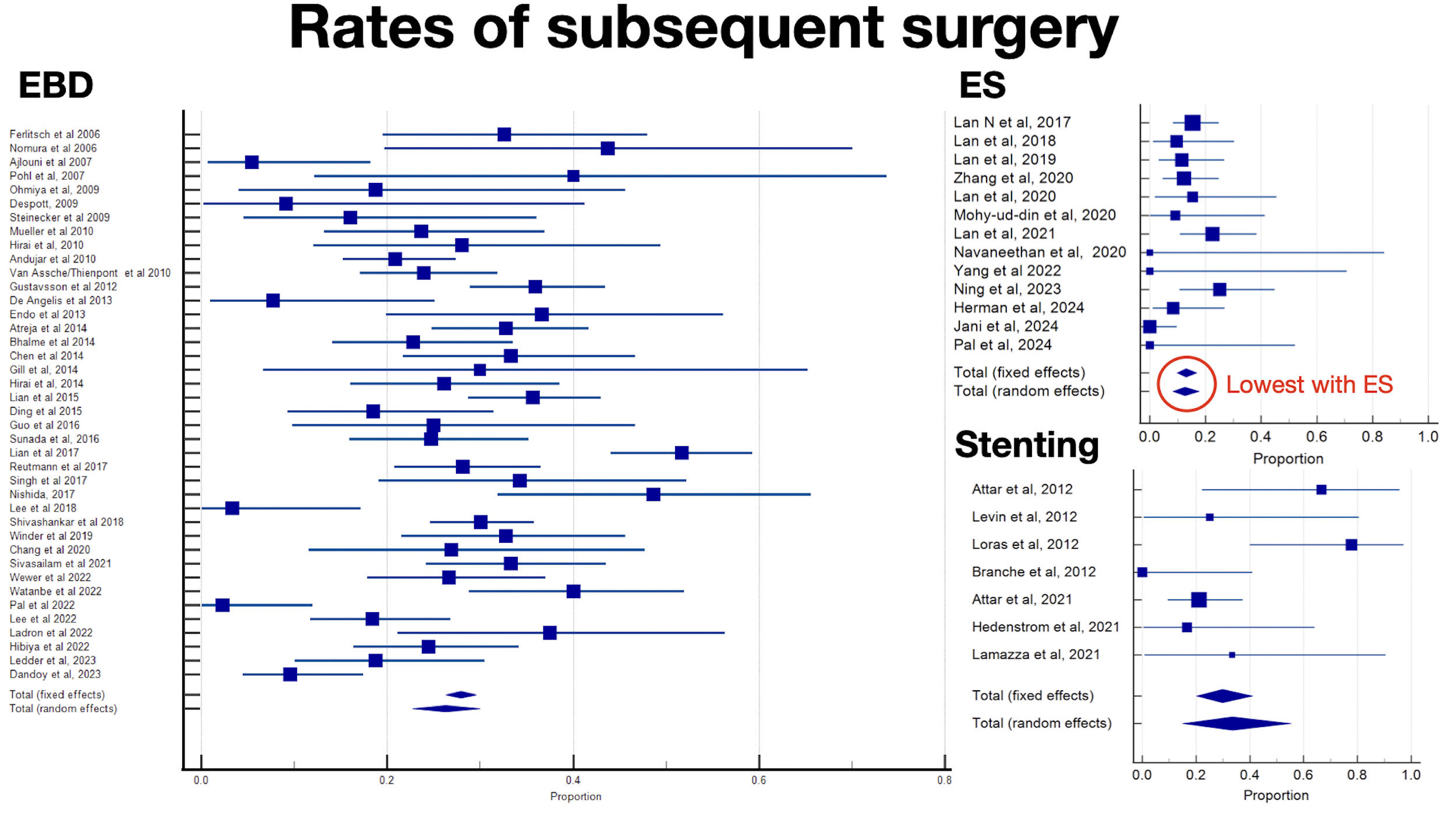
Results: Data from 3,893 patients across 69 studies (43 EBD, 14 ES, 12 stenting) were analyzed (table 1). ES had the highest technical success rate (98.2%), followed by stenting (95.1%) and EBD (89%; p< 0.001). Immediate clinical success was highest with EBD (80.8%), then stenting (69.2%) and ES (65.4%; p< 0.001). EBD had the lowest adverse event rate (4%) compared to ES (5.7%) and stenting (25.7%; p< 0.001). Stenting had the lowest re-intervention rate (36.6%) compared to ES (46.1%) and EBD (59.5%) (p=0.18). ES achieved the lowest surgery rates (12.6%) compared to EBD (26.3%) and stenting (33.5%) (p< 0.001) (Figure 1). Stenting showed high rates of spontaneous (41%) and proximal (9%) migration. No publication bias was detected based on funnel plot evaluations.
Discussion: ES demonstrates the highest technical success and surgery-free survival rates, making it the most effective option. EBD achieves the best immediate clinical outcomes with the fewest complications but higher re-intervention and surgery rates. Although stenting has a lower re-intervention rate, this difference is not statistically significant and it is associated with high migration rates. Further head-to-head randomized trials are needed to provide definitive evidence on the comparative efficacy and safety of these endoscopic treatments.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Partha Pal, MD1, Rajesh Gupta, MD, DM1, Manu Tandan, MD, DM1, D Nageshwar Reddy, MD, DM, FACG1, Gursimran S. Kochhar, MD2. P2661 - Endoscopic Showdown: Balloon Dilation vs Stricturotomy vs Stenting for Inflammatory Bowel Disease Strictures - A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Asian Institute of Gastroenterology, Hyderabad, Telangana, India; 2Allegheny General Hospital, Pittsburgh, PA
Introduction: Resection for inflammatory bowel disease (IBD) strictures carries risks of morbidity, recurrence, and short bowel syndrome. Endoscopic therapies like balloon dilation (EBD), stenting, and stricturotomy (ES) offer alternative treatments with varying success, re-intervention needs, and adverse effects. However, prospective comparative studies on these techniques are lacking, necessitating further research to guide clinical practice.
Methods: A literature search was conducted using PubMed and Embase, spanning 1985 to May 2024. This meta-analysis focused on primary outcomes—clinical success and secondary outcomes including technical succes, adverse events, re-intervention, and need for surgery. Analyses were performed using MedCalc,v22.
Results: Data from 3,893 patients across 69 studies (43 EBD, 14 ES, 12 stenting) were analyzed (table 1). ES had the highest technical success rate (98.2%), followed by stenting (95.1%) and EBD (89%; p< 0.001). Immediate clinical success was highest with EBD (80.8%), then stenting (69.2%) and ES (65.4%; p< 0.001). EBD had the lowest adverse event rate (4%) compared to ES (5.7%) and stenting (25.7%; p< 0.001). Stenting had the lowest re-intervention rate (36.6%) compared to ES (46.1%) and EBD (59.5%) (p=0.18). ES achieved the lowest surgery rates (12.6%) compared to EBD (26.3%) and stenting (33.5%) (p< 0.001) (Figure 1). Stenting showed high rates of spontaneous (41%) and proximal (9%) migration. No publication bias was detected based on funnel plot evaluations.
Discussion: ES demonstrates the highest technical success and surgery-free survival rates, making it the most effective option. EBD achieves the best immediate clinical outcomes with the fewest complications but higher re-intervention and surgery rates. Although stenting has a lower re-intervention rate, this difference is not statistically significant and it is associated with high migration rates. Further head-to-head randomized trials are needed to provide definitive evidence on the comparative efficacy and safety of these endoscopic treatments.
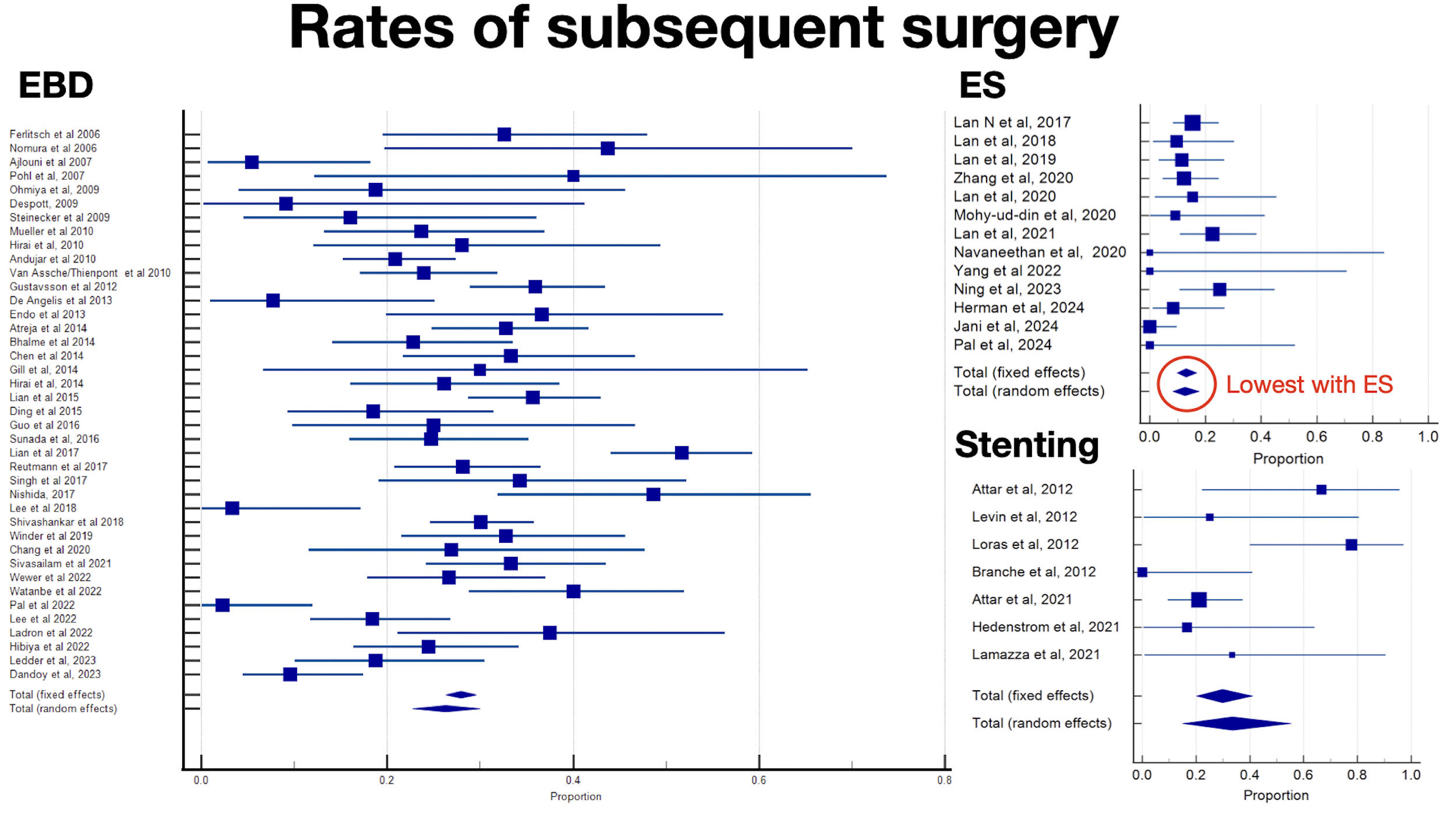
Figure: Meta-analysis showing rates of subesequent surgery wih various endoscopic modalities of stricture treatment in inflammatory bowel disease
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Partha Pal indicated no relevant financial relationships.
Rajesh Gupta indicated no relevant financial relationships.
Manu Tandan indicated no relevant financial relationships.
D Nageshwar Reddy indicated no relevant financial relationships.
Gursimran Kochhar: Boston Scientific Endoscopy – Consultant. DigbI – Stock Options. Eli Lilli – Advisory Committee/Board Member, Speakers Bureau. Olympus Endoscopy – Consultant. Pentax Endoscopy – Consultant. Takeda – Consultant.
Partha Pal, MD1, Rajesh Gupta, MD, DM1, Manu Tandan, MD, DM1, D Nageshwar Reddy, MD, DM, FACG1, Gursimran S. Kochhar, MD2. P2661 - Endoscopic Showdown: Balloon Dilation vs Stricturotomy vs Stenting for Inflammatory Bowel Disease Strictures - A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
