Monday Poster Session
Category: IBD
P2667 - Adherence to Recommended Vaccines Among Individuals With Inflammatory Bowel Disease: Experiences From a Network of Resident Clinics
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Thilini Delungahawatta, MD
MedStar Health
Baltimore, MD
Presenting Author(s)
Thilini Delungahawatta, MD1, Julie Suh, BS2, Joseph Atarere, MD, MPH3, Jasmine Barrow, MD4, Christopher Haas, MD, PhD1, Haider A. Naqvi, MD5
1MedStar Health, Baltimore, MD; 2Georgetown University, Washington, DC; 3MedStar Union Memorial Hospital, Baltimore, MD; 4MedStar Franklin Square Medical Center, Baltimore, MD; 5MedStar Franklin Square Medical Center, Rossville, MD
Introduction: Inflammatory bowel disease (IBD) is an immune-mediated inflammatory condition affecting 1.3% of the U.S. population. Due to dysregulated immune responses and frequent use of immunosuppressive therapies, IBD patients are susceptible to opportunistic infections. Despite established vaccination guidelines for infection prevention in this population, vaccination rates among IBD patients remain suboptimal.
Methods: We conducted a mixed-methods cross-sectional study on adults with an ICD-10 diagnosis of IBD at six internal and family medicine residency clinics in Baltimore, from June 2020 to December 2022. Data collection occurred in two stages between June 2023 to January 2024. In the first stage, demographic and relevant data were abstracted from electronic medical records, and in the second stage, participants not up to date with recommended vaccines were contacted to collect information on reasons for non-adherence.
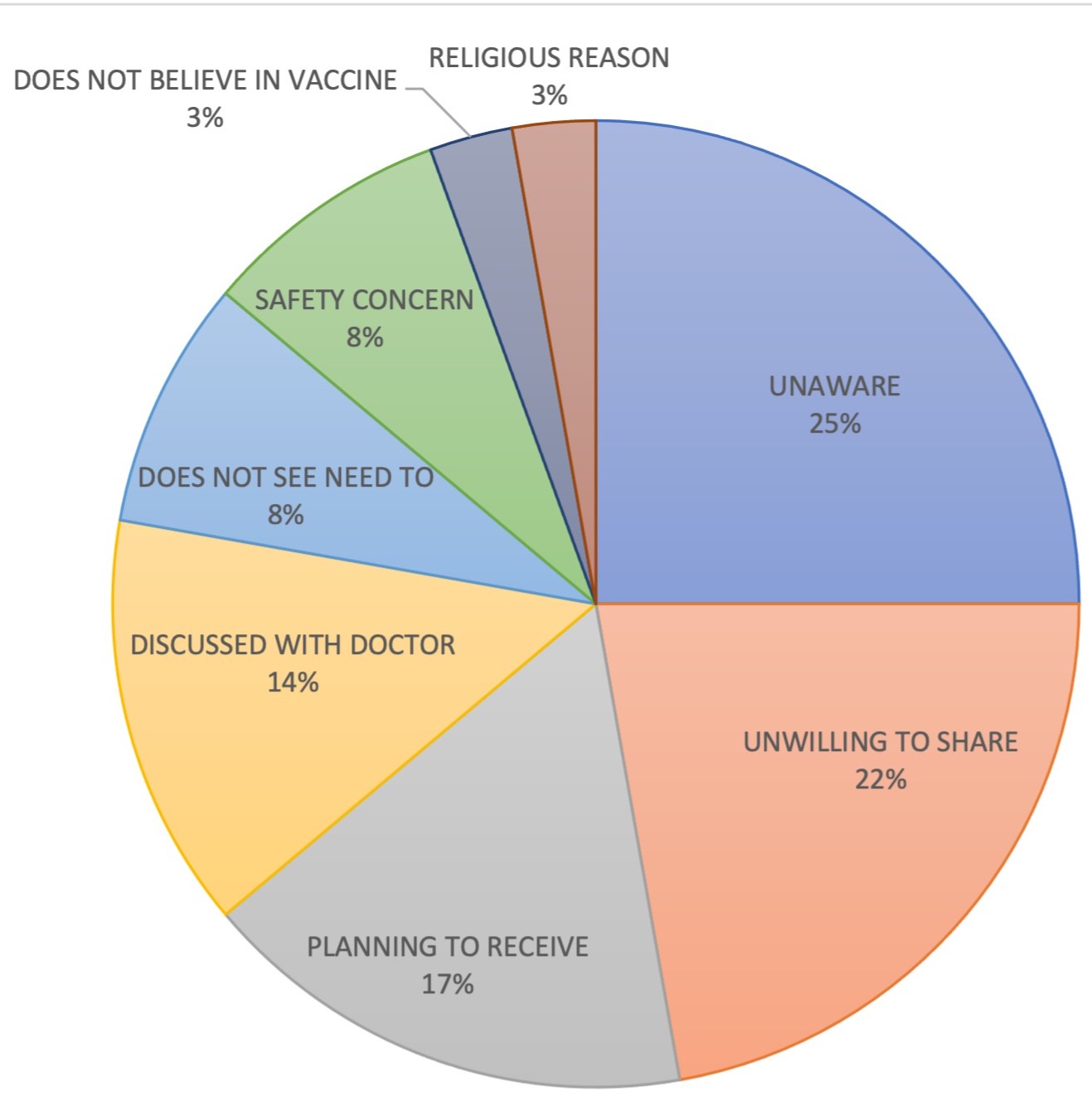
Results: Among the 110 IBD patients studied, 75 had Crohn’s disease (CD) and 35 had Ulcerative Colitis (UC), with majority being female and average age of 48 years; 34.9% were Black. Over two-fifths were currently using at least one immunosuppressive medication. About 73.3% had received at least one influenza vaccination, with UC patients being more likely than CD patients to be up to date with influenza vaccination (60.0% vs 32.9%). For DTaP vaccination, 74.3% of patients were up to date and only 11.9% had not received the vaccine. Hepatitis B vaccination rates were low, with 74.6% not having received the vaccine and only 13.6% completing the three-dose series. COVID-19 vaccination adherence showed that 12.1% of patients did not receive any doses, while 55.0% had received two doses and a booster. Missingness in data was >20% for other recommended vaccinations. After adjusting for age, patients on immunosuppressive medications were more likely to be up to date with influenza [OR 3.25, 95% CI (1.27, 8.30)] and COVID-19 vaccinations [OR 2.64, 95% CI (1.09, 6.37)]. Of the 36 respondents included in the second stage, 25% were unaware of the need for vaccination, 22.2% did not share their reasons for non-adherence, 17% planned to get vaccinated and 8% cited safety concerns.
Discussion: Although influenza and DTaP vaccination rates were comparatively elevated, significant gaps persist in adherence to vaccination guidelines among individuals with IBD. The findings demonstrate a need to prioritize educational interventions targeting both patients and providers.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Thilini Delungahawatta, MD1, Julie Suh, BS2, Joseph Atarere, MD, MPH3, Jasmine Barrow, MD4, Christopher Haas, MD, PhD1, Haider A. Naqvi, MD5. P2667 - Adherence to Recommended Vaccines Among Individuals With Inflammatory Bowel Disease: Experiences From a Network of Resident Clinics, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1MedStar Health, Baltimore, MD; 2Georgetown University, Washington, DC; 3MedStar Union Memorial Hospital, Baltimore, MD; 4MedStar Franklin Square Medical Center, Baltimore, MD; 5MedStar Franklin Square Medical Center, Rossville, MD
Introduction: Inflammatory bowel disease (IBD) is an immune-mediated inflammatory condition affecting 1.3% of the U.S. population. Due to dysregulated immune responses and frequent use of immunosuppressive therapies, IBD patients are susceptible to opportunistic infections. Despite established vaccination guidelines for infection prevention in this population, vaccination rates among IBD patients remain suboptimal.
Methods: We conducted a mixed-methods cross-sectional study on adults with an ICD-10 diagnosis of IBD at six internal and family medicine residency clinics in Baltimore, from June 2020 to December 2022. Data collection occurred in two stages between June 2023 to January 2024. In the first stage, demographic and relevant data were abstracted from electronic medical records, and in the second stage, participants not up to date with recommended vaccines were contacted to collect information on reasons for non-adherence.
Results: Among the 110 IBD patients studied, 75 had Crohn’s disease (CD) and 35 had Ulcerative Colitis (UC), with majority being female and average age of 48 years; 34.9% were Black. Over two-fifths were currently using at least one immunosuppressive medication. About 73.3% had received at least one influenza vaccination, with UC patients being more likely than CD patients to be up to date with influenza vaccination (60.0% vs 32.9%). For DTaP vaccination, 74.3% of patients were up to date and only 11.9% had not received the vaccine. Hepatitis B vaccination rates were low, with 74.6% not having received the vaccine and only 13.6% completing the three-dose series. COVID-19 vaccination adherence showed that 12.1% of patients did not receive any doses, while 55.0% had received two doses and a booster. Missingness in data was >20% for other recommended vaccinations. After adjusting for age, patients on immunosuppressive medications were more likely to be up to date with influenza [OR 3.25, 95% CI (1.27, 8.30)] and COVID-19 vaccinations [OR 2.64, 95% CI (1.09, 6.37)]. Of the 36 respondents included in the second stage, 25% were unaware of the need for vaccination, 22.2% did not share their reasons for non-adherence, 17% planned to get vaccinated and 8% cited safety concerns.
Discussion: Although influenza and DTaP vaccination rates were comparatively elevated, significant gaps persist in adherence to vaccination guidelines among individuals with IBD. The findings demonstrate a need to prioritize educational interventions targeting both patients and providers.
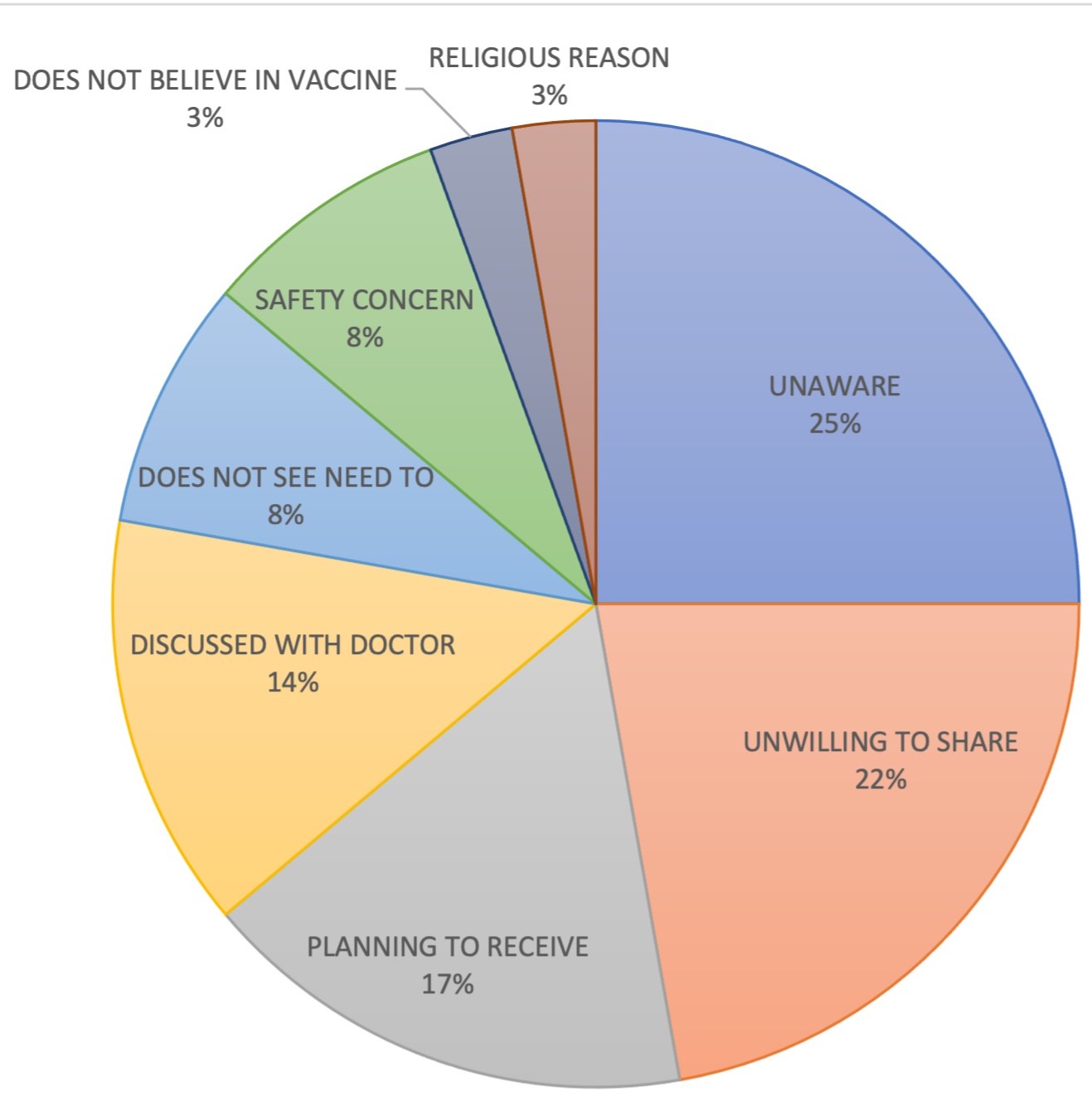
Figure: Reasons provided by patients for non-adherence to vaccination recommendations
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Thilini Delungahawatta indicated no relevant financial relationships.
Julie Suh indicated no relevant financial relationships.
Joseph Atarere indicated no relevant financial relationships.
Jasmine Barrow indicated no relevant financial relationships.
Christopher Haas indicated no relevant financial relationships.
Haider Naqvi indicated no relevant financial relationships.
Thilini Delungahawatta, MD1, Julie Suh, BS2, Joseph Atarere, MD, MPH3, Jasmine Barrow, MD4, Christopher Haas, MD, PhD1, Haider A. Naqvi, MD5. P2667 - Adherence to Recommended Vaccines Among Individuals With Inflammatory Bowel Disease: Experiences From a Network of Resident Clinics, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

