Monday Poster Session
Category: IBD
P2676 - Impact of Vitamin D Deficiency in Ulcerative Colitis Patients: A Nationwide Retrospective Cohort Study
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ahmed Elmoursi, MD, MPH
Harvard Medical School
Lexington, KY
Presenting Author(s)
Ahmed Elmoursi, MD, MPH1, Ahmed Abomhya, MD2, Ibrahim Metawea, MD3, Hazem Abosheaishaa, MD4, Karim Benrajab, MD2, Mostafa Elrazzaz, MD5, Alaa Alareidi, BS2, Mohamed Ali, MS6
1Harvard Medical School, Lexington, KY; 2University of Kentucky, Lexington, KY; 3University of Michigan, Ann Arbor, MI; 4Icahn School of Medicine at Mount Sinai, Queens, NY; 5Detroit Medical Center, Detroit, MI; 6University of Massachusetts Chan Medical School, Boston, KY
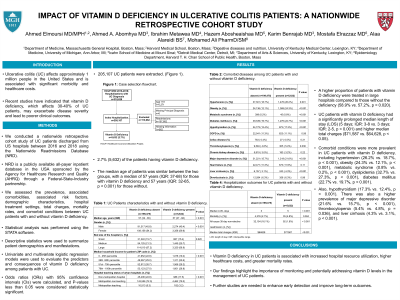
Introduction: Ulcerative colitis (UC) affects approximately 1 million people in the United States and is associated with significant morbidity and healthcare costs. Recent studies have indicated that vitamin D deficiency, which affects 30-40% of UC patients, may exacerbate disease severity and lead to poorer clinical outcomes.
Methods: We conducted a nationwide retrospective cohort study to assess the prevalence, associated risk factors, demographic characteristics, hospital treatment settings, total charges, mortality rates, and comorbid conditions between UC patients with and without vitamin D deficiency.
Results: A total of 205,107 hospital discharges diagnosed with UC were extracted, with 2.7% (5,632) of the patients having vitamin D deficiency. The median age of patients was similar between the two groups, with a median of 57 years (IQR: 37-68) for those with vitamin D deficiency and 57 years (IQR: 32-65, p < 0.001) for those without. A higher proportion of patients with vitamin D deficiency were treated in large hospitals compared to those without the deficiency (58.9% vs. 57.2%, p = 0.020). UC patients with vitamin D deficiency had a significantly prolonged median length of stay (LOS) (5 days; IQR: 3-8 vs. 3 days; IQR: 2-5, p < 0.002) and higher median total charges ($71,587 vs. $64,628, p < 0.05). Patients with vitamin D deficiency had increased mortality rates (4.1% vs. 1.9%, p = 0.004), longer median LOS (7 vs. 5 days, p < 0.001), and greater median total charges ($79,143 vs. $63,683, p < 0.001) than those without vitamin D deficiency. Comorbid conditions were more prevalent in UC patients with vitamin D deficiency, including hypertension (26.2% vs. 18.7%, p < 0.001), obesity (24.3% vs. 12.1%, p < 0.001), metabolic syndrome (0.8% vs. 0.2%, p < 0.001), dyslipidemia (32.7% vs. 27.3%, p < 0.001), diabetes mellitus (22.7% vs. 19.7%, p < 0.001), and hypothyroidism (17.3% vs. 12.4%, p < 0.001). There was also a higher prevalence of major depressive disorder (21.6% vs. 15.7%, p < 0.001), thrombocytopenia (5.4% vs. 4.8%, p = 0.036), and liver cirrhosis (4.3% vs. 3.1%, p < 0.001).
Discussion: Vitamin D deficiency in UC patients is associated with increased hospital resource utilization, higher healthcare costs, and greater mortality rates. Our findings highlight the importance of monitoring and potentially addressing vitamin D levels in the management of UC patients. Further studies are needed to enhance early detection and improve long-term outcomes.
Disclosures:
Ahmed Elmoursi, MD, MPH1, Ahmed Abomhya, MD2, Ibrahim Metawea, MD3, Hazem Abosheaishaa, MD4, Karim Benrajab, MD2, Mostafa Elrazzaz, MD5, Alaa Alareidi, BS2, Mohamed Ali, MS6. P2676 - Impact of Vitamin D Deficiency in Ulcerative Colitis Patients: A Nationwide Retrospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Harvard Medical School, Lexington, KY; 2University of Kentucky, Lexington, KY; 3University of Michigan, Ann Arbor, MI; 4Icahn School of Medicine at Mount Sinai, Queens, NY; 5Detroit Medical Center, Detroit, MI; 6University of Massachusetts Chan Medical School, Boston, KY
Introduction: Ulcerative colitis (UC) affects approximately 1 million people in the United States and is associated with significant morbidity and healthcare costs. Recent studies have indicated that vitamin D deficiency, which affects 30-40% of UC patients, may exacerbate disease severity and lead to poorer clinical outcomes.
Methods: We conducted a nationwide retrospective cohort study to assess the prevalence, associated risk factors, demographic characteristics, hospital treatment settings, total charges, mortality rates, and comorbid conditions between UC patients with and without vitamin D deficiency.
Results: A total of 205,107 hospital discharges diagnosed with UC were extracted, with 2.7% (5,632) of the patients having vitamin D deficiency. The median age of patients was similar between the two groups, with a median of 57 years (IQR: 37-68) for those with vitamin D deficiency and 57 years (IQR: 32-65, p < 0.001) for those without. A higher proportion of patients with vitamin D deficiency were treated in large hospitals compared to those without the deficiency (58.9% vs. 57.2%, p = 0.020). UC patients with vitamin D deficiency had a significantly prolonged median length of stay (LOS) (5 days; IQR: 3-8 vs. 3 days; IQR: 2-5, p < 0.002) and higher median total charges ($71,587 vs. $64,628, p < 0.05). Patients with vitamin D deficiency had increased mortality rates (4.1% vs. 1.9%, p = 0.004), longer median LOS (7 vs. 5 days, p < 0.001), and greater median total charges ($79,143 vs. $63,683, p < 0.001) than those without vitamin D deficiency. Comorbid conditions were more prevalent in UC patients with vitamin D deficiency, including hypertension (26.2% vs. 18.7%, p < 0.001), obesity (24.3% vs. 12.1%, p < 0.001), metabolic syndrome (0.8% vs. 0.2%, p < 0.001), dyslipidemia (32.7% vs. 27.3%, p < 0.001), diabetes mellitus (22.7% vs. 19.7%, p < 0.001), and hypothyroidism (17.3% vs. 12.4%, p < 0.001). There was also a higher prevalence of major depressive disorder (21.6% vs. 15.7%, p < 0.001), thrombocytopenia (5.4% vs. 4.8%, p = 0.036), and liver cirrhosis (4.3% vs. 3.1%, p < 0.001).
Discussion: Vitamin D deficiency in UC patients is associated with increased hospital resource utilization, higher healthcare costs, and greater mortality rates. Our findings highlight the importance of monitoring and potentially addressing vitamin D levels in the management of UC patients. Further studies are needed to enhance early detection and improve long-term outcomes.
Disclosures:
Ahmed Elmoursi indicated no relevant financial relationships.
Ahmed Abomhya indicated no relevant financial relationships.
Ibrahim Metawea indicated no relevant financial relationships.
Hazem Abosheaishaa indicated no relevant financial relationships.
Karim Benrajab indicated no relevant financial relationships.
Mostafa Elrazzaz indicated no relevant financial relationships.
Alaa Alareidi indicated no relevant financial relationships.
Mohamed Ali indicated no relevant financial relationships.
Ahmed Elmoursi, MD, MPH1, Ahmed Abomhya, MD2, Ibrahim Metawea, MD3, Hazem Abosheaishaa, MD4, Karim Benrajab, MD2, Mostafa Elrazzaz, MD5, Alaa Alareidi, BS2, Mohamed Ali, MS6. P2676 - Impact of Vitamin D Deficiency in Ulcerative Colitis Patients: A Nationwide Retrospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
