Monday Poster Session
Category: IBD
P2710 - A Case of Successful FMT Treatment of Recurrent Cdifficile Infection Complicated by Crohn's Disease and Acute Perforated Appendicitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Joshua J. Martin, DO
Loma Linda University Health
Loma Linda, CA
Presenting Author(s)
Joshua J. Martin, DO, Nour Parsa, MD
Loma Linda University Health, Loma Linda, CA
Introduction: Crohn’s disease (CD) is often characterized by chronic transmural inflammation which may involve any portion of the GI tract with stereotypical locations for inflammation in the ileum, cecum, or perianal region.1 When presenting with ileocecal inflammation concerning for flare of known CD, simultaneous appendicitis and acute C diff infection (CDI) must be ruled out as potential mimickers. Although rare, multiple case reports have described patients presenting with right lower quadrant pain in the setting of previous CD diagnoses who were ultimately diagnosed with acute appendicitis.2,3 Alternatively, acute appendicitis can often precede a true diagnosis of Crohn’s. Patients with CD have reported incidence rates of CDI as high as 5-fold higher than the general population making it a prominent cause of acute flares.4
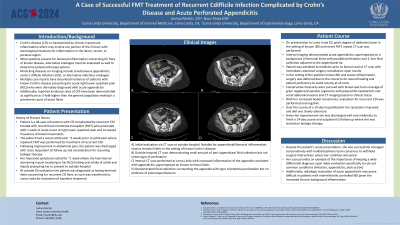
Case Description/Methods: We present the case of a 48 year old woman with CD complicated by recurrent CDI treated with fecal microbiota transplant (FMT) who presented with acute worsening of her symptoms and found to have perforated appendicitis. She presented to the hospital two weeks following inpatient FMT for recurrent CDI. Following her FMT, the patient endorsed significant improvement in both her abdominal pain and frequency of bowel movements; however, she returned to the hospital again following 5 days of worsening right lower quadrant pain different in character compared to her normal IBD flares. Repeat abdominal CT imaging on this admission was now reflective of acute perforated appendicitis with micro abscesses. Both GI and surgery were consulted with recommendations for IV antibiotics and medical management which the patient tolerated. She was able to be transitioned to oral amoxicillin-clavulanic acid and oral diet with plans for outpatient IBD clinic follow up.
Discussion: Despite the patient's acute presentation, she was successfully managed conservatively, with multidisciplinary team consensus to withhold surgical intervention unless her condition worsened. She continued to do well on an outpatient basis. Her case provides an example of the importance of keeping a wide differential diagnosis (infection, appendicitis, obstruction) to distinguish between CD flares and alternative causes of acute abdominal pain in the setting of IBD.
Disclosures:
Joshua J. Martin, DO, Nour Parsa, MD. P2710 - A Case of Successful FMT Treatment of Recurrent Cdifficile Infection Complicated by Crohn's Disease and Acute Perforated Appendicitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Loma Linda University Health, Loma Linda, CA
Introduction: Crohn’s disease (CD) is often characterized by chronic transmural inflammation which may involve any portion of the GI tract with stereotypical locations for inflammation in the ileum, cecum, or perianal region.1 When presenting with ileocecal inflammation concerning for flare of known CD, simultaneous appendicitis and acute C diff infection (CDI) must be ruled out as potential mimickers. Although rare, multiple case reports have described patients presenting with right lower quadrant pain in the setting of previous CD diagnoses who were ultimately diagnosed with acute appendicitis.2,3 Alternatively, acute appendicitis can often precede a true diagnosis of Crohn’s. Patients with CD have reported incidence rates of CDI as high as 5-fold higher than the general population making it a prominent cause of acute flares.4
Case Description/Methods: We present the case of a 48 year old woman with CD complicated by recurrent CDI treated with fecal microbiota transplant (FMT) who presented with acute worsening of her symptoms and found to have perforated appendicitis. She presented to the hospital two weeks following inpatient FMT for recurrent CDI. Following her FMT, the patient endorsed significant improvement in both her abdominal pain and frequency of bowel movements; however, she returned to the hospital again following 5 days of worsening right lower quadrant pain different in character compared to her normal IBD flares. Repeat abdominal CT imaging on this admission was now reflective of acute perforated appendicitis with micro abscesses. Both GI and surgery were consulted with recommendations for IV antibiotics and medical management which the patient tolerated. She was able to be transitioned to oral amoxicillin-clavulanic acid and oral diet with plans for outpatient IBD clinic follow up.
Discussion: Despite the patient's acute presentation, she was successfully managed conservatively, with multidisciplinary team consensus to withhold surgical intervention unless her condition worsened. She continued to do well on an outpatient basis. Her case provides an example of the importance of keeping a wide differential diagnosis (infection, appendicitis, obstruction) to distinguish between CD flares and alternative causes of acute abdominal pain in the setting of IBD.
Disclosures:
Joshua Martin indicated no relevant financial relationships.
Nour Parsa indicated no relevant financial relationships.
Joshua J. Martin, DO, Nour Parsa, MD. P2710 - A Case of Successful FMT Treatment of Recurrent Cdifficile Infection Complicated by Crohn's Disease and Acute Perforated Appendicitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
