Monday Poster Session
Category: IBD
P2735 - Buprenorphine: A Solution to the Negative Effects of Opioids in IBD
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- DR
Daniel J. Rausa, DO
Lenox Hill Hospital, Northwell Health
New York, NY
Presenting Author(s)
Daniel J. Rausa, DO1, Jeremy Polman, DO, MS, MBA1, Benjamin Vipler, MD, MEd2, Anjali Mone, MD1
1Lenox Hill Hospital, Northwell Health, New York, NY; 2University of Colorado Anschutz Medical Campus, Aurora, CO
Introduction: Chronic abdominal pain is a common symptom experienced by patients with Irritable Bowel Disease (IBD). In the absence of markers of inflammation, treatment options are limited. Chronic opioid therapy is often utilized despite literature indicating associated poor long term functional outcomes and gastrointestinal side effects. Here we describe a patient with Crohn’s disease complicated by narcotic bowel syndrome (NBS) and introduce buprenorphine as a treatment option.
Case Description/Methods: A 48-year-old man with bipolar disorder and Crohn’s disease on adalimumab (ADA) presented to the emergency department (ED) for the 26th time over one year with acute worsening of chronic abdominal pain. Previous inpatient therapies included numerous courses of systemic steroids for presumed IBD flares despite lacking markers of inflammation. He also had a complicated procedural history including a proctocolectomy with ileal pouch anal anastomosis and multiple small bowel resections with lysis of adhesions. Given lack of symptomatic improvement, he was prescribed long-term opioid therapy.
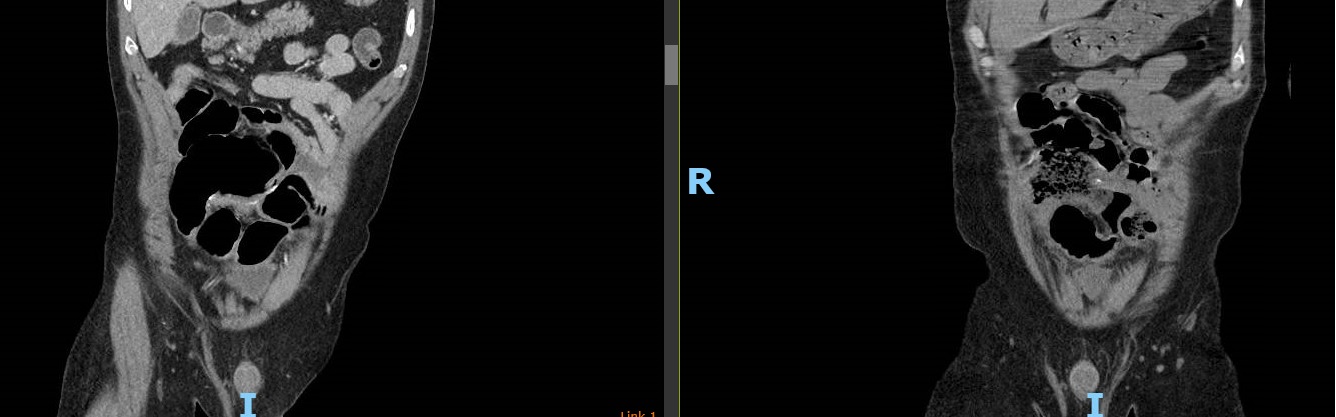
His abdominal pain was diffuse and crampy with associated nausea, though he was passing flatus and stool. Vital signs were normal and his abdomen was soft, non-distended but diffusely tender. Blood tests were unrevealing. ADA level was 6.6ug/ml with undetectable antibodies. Stool testing for infectious pathogens was negative. Computed tomography (CT) of the abdomen and pelvis was stable from prior imaging and showed small bowel dilatation up to 5.2cm at the site of the anastomosis in the mid-lower abdomen without obstruction.
Pouchoscopy revealed patent anastomoses and an area of ileal dilation proximally. Biopsies were unrevealing. NBS was considered and the patient consented for buprenorphine therapy. Within 48 hours of induction, he described significant symptom improvement and was discharged. Over the next 3 months, he reported minimal to no abdominal pain on buprenorphine. A subsequent CT scan revealed improvement of the small bowel dilatation.
Discussion: This case demonstrates the role buprenorphine has in the care of patients with IBD complicated by NBS. Clinical practice updates on NBS emphasize opioid cessation but provide little insight on how to accomplish this. Particularly among patients with IBD, chronic opioid use is associated with more severe IBD and increased healthcare use. As such, buprenorphine is a low-risk therapy that stands to benefit this vulnerable and often marginalized patient population.
Disclosures:
Daniel J. Rausa, DO1, Jeremy Polman, DO, MS, MBA1, Benjamin Vipler, MD, MEd2, Anjali Mone, MD1. P2735 - Buprenorphine: A Solution to the Negative Effects of Opioids in IBD, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Lenox Hill Hospital, Northwell Health, New York, NY; 2University of Colorado Anschutz Medical Campus, Aurora, CO
Introduction: Chronic abdominal pain is a common symptom experienced by patients with Irritable Bowel Disease (IBD). In the absence of markers of inflammation, treatment options are limited. Chronic opioid therapy is often utilized despite literature indicating associated poor long term functional outcomes and gastrointestinal side effects. Here we describe a patient with Crohn’s disease complicated by narcotic bowel syndrome (NBS) and introduce buprenorphine as a treatment option.
Case Description/Methods: A 48-year-old man with bipolar disorder and Crohn’s disease on adalimumab (ADA) presented to the emergency department (ED) for the 26th time over one year with acute worsening of chronic abdominal pain. Previous inpatient therapies included numerous courses of systemic steroids for presumed IBD flares despite lacking markers of inflammation. He also had a complicated procedural history including a proctocolectomy with ileal pouch anal anastomosis and multiple small bowel resections with lysis of adhesions. Given lack of symptomatic improvement, he was prescribed long-term opioid therapy.
His abdominal pain was diffuse and crampy with associated nausea, though he was passing flatus and stool. Vital signs were normal and his abdomen was soft, non-distended but diffusely tender. Blood tests were unrevealing. ADA level was 6.6ug/ml with undetectable antibodies. Stool testing for infectious pathogens was negative. Computed tomography (CT) of the abdomen and pelvis was stable from prior imaging and showed small bowel dilatation up to 5.2cm at the site of the anastomosis in the mid-lower abdomen without obstruction.
Pouchoscopy revealed patent anastomoses and an area of ileal dilation proximally. Biopsies were unrevealing. NBS was considered and the patient consented for buprenorphine therapy. Within 48 hours of induction, he described significant symptom improvement and was discharged. Over the next 3 months, he reported minimal to no abdominal pain on buprenorphine. A subsequent CT scan revealed improvement of the small bowel dilatation.
Discussion: This case demonstrates the role buprenorphine has in the care of patients with IBD complicated by NBS. Clinical practice updates on NBS emphasize opioid cessation but provide little insight on how to accomplish this. Particularly among patients with IBD, chronic opioid use is associated with more severe IBD and increased healthcare use. As such, buprenorphine is a low-risk therapy that stands to benefit this vulnerable and often marginalized patient population.
Figure: Small bowel dilatation pre buprenorphine (left) and 10 months post buprenorphine (right)
Disclosures:
Daniel Rausa indicated no relevant financial relationships.
Jeremy Polman indicated no relevant financial relationships.
Benjamin Vipler indicated no relevant financial relationships.
Anjali Mone indicated no relevant financial relationships.
Daniel J. Rausa, DO1, Jeremy Polman, DO, MS, MBA1, Benjamin Vipler, MD, MEd2, Anjali Mone, MD1. P2735 - Buprenorphine: A Solution to the Negative Effects of Opioids in IBD, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
