Monday Poster Session
Category: IBD
P2739 - A Rare Case of Azathioprine and Infliximab-Induced Pneumonitis and Polymorphic Lymphoproliferative Disorder
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Sarah Dwyer Holland, MD, MS
Brown University
Providence, RI
Presenting Author(s)
Sarah Dwyer Holland, MD, MS1, Yousef Elfanagely, MD1, Amanda Pressman, MD2, Syed Quadri, MD3
1Brown University, Providence, RI; 2Brown University / Warren Alpert Medical School, Providence, RI; 3Brown Medicine/Lifespan, Providence, RI
Introduction: The workup of dyspnea in patients with inflammatory bowel disease (IBD) on immunosuppressive and biologic agents can be complex. We present a case of a patient with ulcerative colitis who developed drug-induced pneumonitis and polymorphic lymphoproliferative disorder after initiating azathioprine and infliximab.
Case Description/Methods: A 47-year-old female with a five-year history of pan-ulcerative colitis on adalimumab presented to establish care. Labs showed an anti-adalimumab antibody level of 112, a low drug level of 3.8, and fecal calprotectin 62.4. Colonoscopy showed Mayo Score 3 pancolitis with pathology showing severely active colitis. She was taken off adalimumab and transitioned to infliximab and azathioprine.
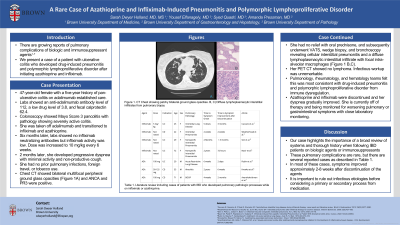
Labs six months later showed no infliximab neutralizing antibodies, but infliximab activity was low. Infliximab was increased to 10 mg/kg every 6 weeks. Two months later, she developed progressive dyspnea with minimal activity and non-productive cough. She had no prior pulmonary infections, foreign travel, or tobacco use. Chest CT showed bilateral multifocal peripheral ground glass opacities and pulmonary function testing showed a restrictive pattern with reduced DLCO (Figure 1A). ANCA and PR3 were positive. She had no relief with oral prednisone, and subsequently underwent VATS, wedge biopsy, and bronchoscopy revealing cellular interstitial pneumonitis and a diffuse lymphoplasmacytic interstitial infiltrate with focal intra-alveolar macrophages (Figure 1 B,C). Her PET CT showed no lymphoma. Infectious workup was unremarkable.
Pulmonology and hematology teams felt this was most consistent with drug-induced pneumonitis and polymorphic lymphoproliferative disorder from immune dysregulation. Azathioprine and infliximab were discontinued and her dyspnea gradually improved. She is currently off of therapy and being monitored for worsening pulmonary or gastrointestinal symptoms with close laboratory monitoring.
Discussion: Workup of pulmonary symptoms in patients with IBD requires a thoughtful approach, including evaluation for worsening GI symptoms consistent with a flare. For patients on a biologic agent or immunosuppressant, infectious etiologies must be ruled out before considering a primary process or secondary process from medication. These non-infectious causes of pulmonary complications are rare, but there are several reported cases (Table 1). Our case highlights the importance of a broad review of systems and thorough history when following IBD patients on these agents.

Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sarah Dwyer Holland, MD, MS1, Yousef Elfanagely, MD1, Amanda Pressman, MD2, Syed Quadri, MD3. P2739 - A Rare Case of Azathioprine and Infliximab-Induced Pneumonitis and Polymorphic Lymphoproliferative Disorder, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Brown University, Providence, RI; 2Brown University / Warren Alpert Medical School, Providence, RI; 3Brown Medicine/Lifespan, Providence, RI
Introduction: The workup of dyspnea in patients with inflammatory bowel disease (IBD) on immunosuppressive and biologic agents can be complex. We present a case of a patient with ulcerative colitis who developed drug-induced pneumonitis and polymorphic lymphoproliferative disorder after initiating azathioprine and infliximab.
Case Description/Methods: A 47-year-old female with a five-year history of pan-ulcerative colitis on adalimumab presented to establish care. Labs showed an anti-adalimumab antibody level of 112, a low drug level of 3.8, and fecal calprotectin 62.4. Colonoscopy showed Mayo Score 3 pancolitis with pathology showing severely active colitis. She was taken off adalimumab and transitioned to infliximab and azathioprine.
Labs six months later showed no infliximab neutralizing antibodies, but infliximab activity was low. Infliximab was increased to 10 mg/kg every 6 weeks. Two months later, she developed progressive dyspnea with minimal activity and non-productive cough. She had no prior pulmonary infections, foreign travel, or tobacco use. Chest CT showed bilateral multifocal peripheral ground glass opacities and pulmonary function testing showed a restrictive pattern with reduced DLCO (Figure 1A). ANCA and PR3 were positive. She had no relief with oral prednisone, and subsequently underwent VATS, wedge biopsy, and bronchoscopy revealing cellular interstitial pneumonitis and a diffuse lymphoplasmacytic interstitial infiltrate with focal intra-alveolar macrophages (Figure 1 B,C). Her PET CT showed no lymphoma. Infectious workup was unremarkable.
Pulmonology and hematology teams felt this was most consistent with drug-induced pneumonitis and polymorphic lymphoproliferative disorder from immune dysregulation. Azathioprine and infliximab were discontinued and her dyspnea gradually improved. She is currently off of therapy and being monitored for worsening pulmonary or gastrointestinal symptoms with close laboratory monitoring.
Discussion: Workup of pulmonary symptoms in patients with IBD requires a thoughtful approach, including evaluation for worsening GI symptoms consistent with a flare. For patients on a biologic agent or immunosuppressant, infectious etiologies must be ruled out before considering a primary process or secondary process from medication. These non-infectious causes of pulmonary complications are rare, but there are several reported cases (Table 1). Our case highlights the importance of a broad review of systems and thorough history when following IBD patients on these agents.

Figure: Figure 1. A) CT Chest showing patchy bilateral ground glass opacities. B, C) Diffuse lymphoplasmacytic interstitial infiltrates from pulmonary biopsy.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sarah Dwyer Holland indicated no relevant financial relationships.
Yousef Elfanagely indicated no relevant financial relationships.
Amanda Pressman indicated no relevant financial relationships.
Syed Quadri indicated no relevant financial relationships.
Sarah Dwyer Holland, MD, MS1, Yousef Elfanagely, MD1, Amanda Pressman, MD2, Syed Quadri, MD3. P2739 - A Rare Case of Azathioprine and Infliximab-Induced Pneumonitis and Polymorphic Lymphoproliferative Disorder, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
