Monday Poster Session
Category: Interventional Endoscopy
P2746 - Endoscopic Bariatric Therapies Are Associated With a Reduction in Noninvasive Measures of Hepatic Steatosis in Patients With Obesity
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AH
Alyssar Habib, MD
NYU Grossman School of Medicine
New York, NY
Presenting Author(s)
Khalid Fahoum, MD, MSc1, Alyssar Habib, MD1, Sharnendra Sidhu, MD1, Sigrid Young, MD1, Leah Kim, MD2, Violeta Popov, MD, PhD2
1NYU Grossman School of Medicine, New York, NY; 2NYU Langone Health, New York, NY
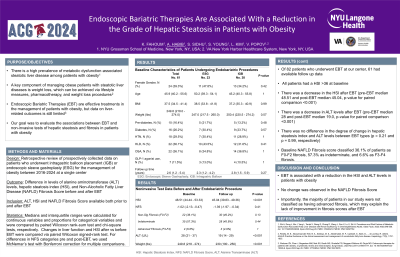
Introduction: There is a high prevalence of metabolic dysfunction-associated steatotic liver disease among patients with obesity. A key component of managing these patients is weight loss, which can be achieved via lifestyle measures, pharmacotherapy, and weight loss procedures. Endoscopic bariatric therapies (EBT) are effective treatments in the management of patients with obesity, but data on liver-related outcomes is still limited. Our goal was to evaluate the associations between EBT and noninvasive tests of hepatic steatosis and fibrosis in patients with obesity.
Methods: Patients who underwent intragastric balloon placement or endoscopic sleeve gastroplasty for the management of obesity between 2016-2024 at a single center were included. Patients without available follow up laboratory and anthropometric data in the electronic medical record were excluded. The primary outcome was the difference in levels of alanine aminotransferase (ALT) levels, hepatic steatosis index (HSI), and Non-Alcoholic Fatty Liver Disease (NAFLD) Fibrosis score before and after EBT, assessed using the paired Wilcoxon signed-rank test.
Results: Of 82 patients who underwent EBT at our center, 62 had available follow up data. The median baseline BMI was 37.4 (interquartile range – IQR of 34.6-41.3) and median baseline weight was 250 lb (IQR 219 – 274 lb). The patients were 38.7% female and the median age was 45.6 (IQR 40.2 – 55.3). There was a median weight loss of 20.3 lb (IQR 7.6 – 37.8) over a median of 2.4 years (IQR 1.7-4.1). There was a decrease in the HSI after EBT (pre-EBT median 48.8 and post-EBT median 45.3, p-value for paired comparison < 0.0001). Similarly, there was a decrease in ALT levels after EBT (pre-EBT median 28.5 and post-EBT median 19.0, p-value for paired comparison < 0.0001). There was no difference in the degree of change in hepatic steatosis index and ALT levels between EBT types (p = 0.21 and p = 0.97, respectively). Baseline NAFLD Fibrosis score classified 37% of patients as F0-F2 fibrosis, 56% as indeterminate, and 6% as F3-F4 fibrosis. There was no change in the NAFLD Fibrosis score after EBT (p-value for paired comparison 0.41).
Discussion: EBT is associated with a reduction in the HSI and ALT levels in patients with obesity, with no change observed in the NAFLD Fibrosis score. The majority of patients in our study were not classified as having advanced fibrosis, which may explain the lack of improvement in fibrosis scores after EBT.
Disclosures:
Khalid Fahoum, MD, MSc1, Alyssar Habib, MD1, Sharnendra Sidhu, MD1, Sigrid Young, MD1, Leah Kim, MD2, Violeta Popov, MD, PhD2. P2746 - Endoscopic Bariatric Therapies Are Associated With a Reduction in Noninvasive Measures of Hepatic Steatosis in Patients With Obesity, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1NYU Grossman School of Medicine, New York, NY; 2NYU Langone Health, New York, NY
Introduction: There is a high prevalence of metabolic dysfunction-associated steatotic liver disease among patients with obesity. A key component of managing these patients is weight loss, which can be achieved via lifestyle measures, pharmacotherapy, and weight loss procedures. Endoscopic bariatric therapies (EBT) are effective treatments in the management of patients with obesity, but data on liver-related outcomes is still limited. Our goal was to evaluate the associations between EBT and noninvasive tests of hepatic steatosis and fibrosis in patients with obesity.
Methods: Patients who underwent intragastric balloon placement or endoscopic sleeve gastroplasty for the management of obesity between 2016-2024 at a single center were included. Patients without available follow up laboratory and anthropometric data in the electronic medical record were excluded. The primary outcome was the difference in levels of alanine aminotransferase (ALT) levels, hepatic steatosis index (HSI), and Non-Alcoholic Fatty Liver Disease (NAFLD) Fibrosis score before and after EBT, assessed using the paired Wilcoxon signed-rank test.
Results: Of 82 patients who underwent EBT at our center, 62 had available follow up data. The median baseline BMI was 37.4 (interquartile range – IQR of 34.6-41.3) and median baseline weight was 250 lb (IQR 219 – 274 lb). The patients were 38.7% female and the median age was 45.6 (IQR 40.2 – 55.3). There was a median weight loss of 20.3 lb (IQR 7.6 – 37.8) over a median of 2.4 years (IQR 1.7-4.1). There was a decrease in the HSI after EBT (pre-EBT median 48.8 and post-EBT median 45.3, p-value for paired comparison < 0.0001). Similarly, there was a decrease in ALT levels after EBT (pre-EBT median 28.5 and post-EBT median 19.0, p-value for paired comparison < 0.0001). There was no difference in the degree of change in hepatic steatosis index and ALT levels between EBT types (p = 0.21 and p = 0.97, respectively). Baseline NAFLD Fibrosis score classified 37% of patients as F0-F2 fibrosis, 56% as indeterminate, and 6% as F3-F4 fibrosis. There was no change in the NAFLD Fibrosis score after EBT (p-value for paired comparison 0.41).
Discussion: EBT is associated with a reduction in the HSI and ALT levels in patients with obesity, with no change observed in the NAFLD Fibrosis score. The majority of patients in our study were not classified as having advanced fibrosis, which may explain the lack of improvement in fibrosis scores after EBT.
Disclosures:
Khalid Fahoum indicated no relevant financial relationships.
Alyssar Habib indicated no relevant financial relationships.
Sharnendra Sidhu indicated no relevant financial relationships.
Sigrid Young indicated no relevant financial relationships.
Leah Kim indicated no relevant financial relationships.
Violeta Popov: MicroTech Endoscopy – Grant/Research Support.
Khalid Fahoum, MD, MSc1, Alyssar Habib, MD1, Sharnendra Sidhu, MD1, Sigrid Young, MD1, Leah Kim, MD2, Violeta Popov, MD, PhD2. P2746 - Endoscopic Bariatric Therapies Are Associated With a Reduction in Noninvasive Measures of Hepatic Steatosis in Patients With Obesity, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
