Monday Poster Session
Category: Interventional Endoscopy
P2748 - Risk Prediction for Early Postoperative Bleeding in Endoscopic Sleeve Gastroplasty: Development and Internal Validation of a Logistic Regression-Based Scoring System
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- GN
Gul Nawaz, MD
Marshfield Medical Center
Marshfield, WI
Presenting Author(s)
Faisal Inayat, MBBS1, Muhammad Sajeel Anwar, MD2, Gul Nawaz, MD3, Ahtshamullah Chaudhry, MD4, Faisal Ibrahim, MBBS5, Hassam Ali, MD6
1Allama Iqbal Medical College, Lahore, Punjab, Pakistan; 2UHS Wilson Medical Center, Johnson City, NY; 3Marshfield Medical Center, Marshfield, WI; 4St. Dominic's Hospital, Jackson, MS; 5Wexham Park Hospital, Slough, England, United Kingdom; 6East Carolina University Brody School of Medicine, Greenville, NC
Introduction: Gastrointestinal (GI) bleeding is a rare but important complication of endoscopic sleeve gastroplasty (ESG). Patients frequently express concerns about the likelihood of experiencing postprocedure GI bleeding. Despite the pressing need, no scoring systems are specifically designed to predict low-risk post-ESG patients. Supervised machine learning may offer a promising avenue for accurately categorizing the procedural risk profiles. We aim to develop and internally validate a scoring system determining the individualized risk of GI bleeding within the first 30 days after ESG.
Methods: Using the 2016-2021 Metabolic and Bariatric Surgery Accreditation Quality Improvement Program (MBSAQIP) database, 1,624 patients who underwent ESG were identified. Stepwise multivariate logistic regression was utilized to select the most promising predictors of GI bleeding following ESG within 30 days. The regression coefficients of predictive variables selected by stepwise regression were used to develop an algorithm. The algorithm's performance was assessed using receiver operator curves by 5-fold cross-validation.
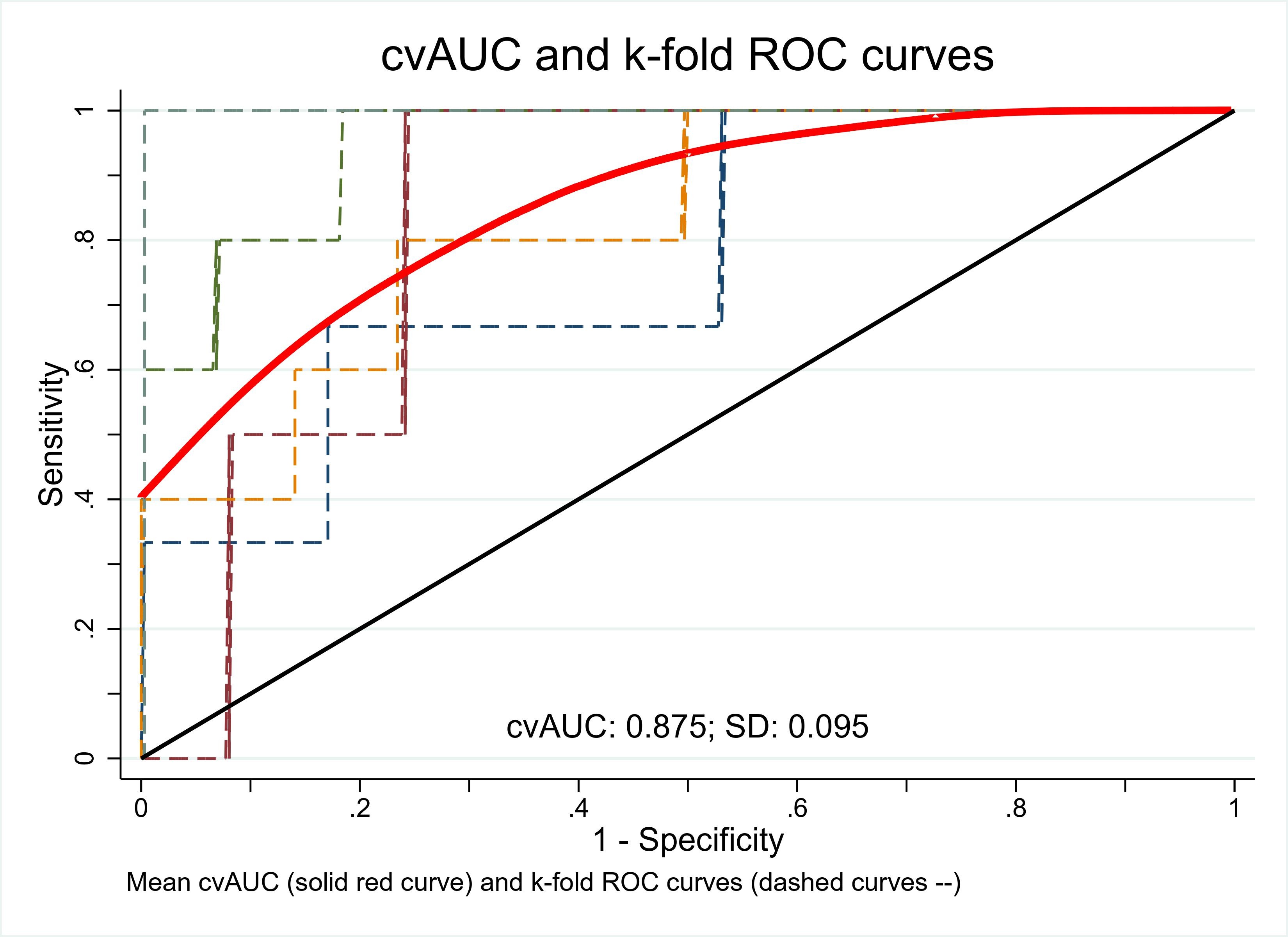
Results: Stepwise multivariate logistic regression selected five of the 26 initial variables assessed with a P value < 0.05. These were female gender with an odds ratio (OR) of 0.22 (P = 0.008), preoperative weight (lbs) (OR 1.02, P < 0.001), hypertension (OR 0.14, P = 0.003), hyperlipidemia (OR 5.60, P = 0.005), and previous foregut surgery (OR 5.67, P = 0.009). In the logistic regression model, these variables were weighted based on their regression coefficients. For the risk model, an algorithm was subsequently developed. The cutoff score was established by the Youden index at 4.12; scores below this value were classified as having a low risk of bleeding following ESG. The area under the curve (AUC) for the risk model was determined to be 0.88 (95%CI: 0.72-0.93) (Figure 1). This resulted in sensitivity and specificity of 88.2% and 70.8%, respectively.
Discussion: This is the first population-based study that successfully developed and validated a scoring system predicting the risk of GI bleeding within 30 days post-ESG. The excellent discriminatory power of our risk assessment tool demonstrated its accuracy in predicting person-specific risk of gastrointestinal bleeding within the first 30 days post-ESG. This scoring system could prove to be a helpful tool for clinicians in determining which patients would benefit from targeted monitoring and therapy.
Disclosures:
Faisal Inayat, MBBS1, Muhammad Sajeel Anwar, MD2, Gul Nawaz, MD3, Ahtshamullah Chaudhry, MD4, Faisal Ibrahim, MBBS5, Hassam Ali, MD6. P2748 - Risk Prediction for Early Postoperative Bleeding in Endoscopic Sleeve Gastroplasty: Development and Internal Validation of a Logistic Regression-Based Scoring System, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Allama Iqbal Medical College, Lahore, Punjab, Pakistan; 2UHS Wilson Medical Center, Johnson City, NY; 3Marshfield Medical Center, Marshfield, WI; 4St. Dominic's Hospital, Jackson, MS; 5Wexham Park Hospital, Slough, England, United Kingdom; 6East Carolina University Brody School of Medicine, Greenville, NC
Introduction: Gastrointestinal (GI) bleeding is a rare but important complication of endoscopic sleeve gastroplasty (ESG). Patients frequently express concerns about the likelihood of experiencing postprocedure GI bleeding. Despite the pressing need, no scoring systems are specifically designed to predict low-risk post-ESG patients. Supervised machine learning may offer a promising avenue for accurately categorizing the procedural risk profiles. We aim to develop and internally validate a scoring system determining the individualized risk of GI bleeding within the first 30 days after ESG.
Methods: Using the 2016-2021 Metabolic and Bariatric Surgery Accreditation Quality Improvement Program (MBSAQIP) database, 1,624 patients who underwent ESG were identified. Stepwise multivariate logistic regression was utilized to select the most promising predictors of GI bleeding following ESG within 30 days. The regression coefficients of predictive variables selected by stepwise regression were used to develop an algorithm. The algorithm's performance was assessed using receiver operator curves by 5-fold cross-validation.
Results: Stepwise multivariate logistic regression selected five of the 26 initial variables assessed with a P value < 0.05. These were female gender with an odds ratio (OR) of 0.22 (P = 0.008), preoperative weight (lbs) (OR 1.02, P < 0.001), hypertension (OR 0.14, P = 0.003), hyperlipidemia (OR 5.60, P = 0.005), and previous foregut surgery (OR 5.67, P = 0.009). In the logistic regression model, these variables were weighted based on their regression coefficients. For the risk model, an algorithm was subsequently developed. The cutoff score was established by the Youden index at 4.12; scores below this value were classified as having a low risk of bleeding following ESG. The area under the curve (AUC) for the risk model was determined to be 0.88 (95%CI: 0.72-0.93) (Figure 1). This resulted in sensitivity and specificity of 88.2% and 70.8%, respectively.
Discussion: This is the first population-based study that successfully developed and validated a scoring system predicting the risk of GI bleeding within 30 days post-ESG. The excellent discriminatory power of our risk assessment tool demonstrated its accuracy in predicting person-specific risk of gastrointestinal bleeding within the first 30 days post-ESG. This scoring system could prove to be a helpful tool for clinicians in determining which patients would benefit from targeted monitoring and therapy.
Figure: Figure 1. Receiver operating characteristic (ROC) curve with mean cross-validated area under the curve (CvAUC) after 5-fold cross-validation. Area under the curve (AUC): 0.88 (boot strapped bias corrected 95% confidence interval: 0.72-0.93).
Disclosures:
Faisal Inayat indicated no relevant financial relationships.
Muhammad Sajeel Anwar indicated no relevant financial relationships.
Gul Nawaz indicated no relevant financial relationships.
Ahtshamullah Chaudhry indicated no relevant financial relationships.
Faisal Ibrahim indicated no relevant financial relationships.
Hassam Ali indicated no relevant financial relationships.
Faisal Inayat, MBBS1, Muhammad Sajeel Anwar, MD2, Gul Nawaz, MD3, Ahtshamullah Chaudhry, MD4, Faisal Ibrahim, MBBS5, Hassam Ali, MD6. P2748 - Risk Prediction for Early Postoperative Bleeding in Endoscopic Sleeve Gastroplasty: Development and Internal Validation of a Logistic Regression-Based Scoring System, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
