Monday Poster Session
Category: Interventional Endoscopy
P2751 - Role of Statins in Preventing Post ERCP Pancreatitis: Insights From a Retrospective Study
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SS
Sohaib Shabih, MD
Guthrie Robert Packer Hospital
Sayre, PA
Presenting Author(s)
Sohaib Shabih, MD1, Daebin Im, MD, MPH1, Subash Ghimire, MD1, Amlish Gondal, MD1, Rasmita Budhathoki, MD1, Tsu Jung Yang, MD1, Madeline Mylod, MS2, Vivian Deng, MS2, Noah West, MS2, Conor Banta, 3, Michael Georgetson, MD1, Thomas McDonald, MD1
1Guthrie Robert Packer Hospital, Sayre, PA; 2Lake Erie College of Osteopathic Medicine, Sayre, PA; 3Geisinger Commonwealth School of Medicine, Sayre, PA
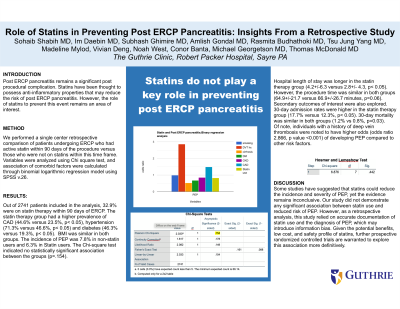
Introduction: Post Endoscopic Retrograde Cholangiopancreatography (ERCP) pancreatitis (PEP) remains a significant post procedural complication. Statins have been thought to possess anti-inflammatory properties that may reduce the incidence of PEP. However, the role of Statins to prevent this event remains an area of interest.
Methods: We performed a single center retrospective comparison of patients undergoing ERCP who had active statin prescription within 90 days of the procedure versus those who were not on statins within this time frame. Variables were analyzed using Chi square test and association of comorbid conditions were calculated through binomial logarithmic regression model using SPSS v.26
Results: Out of 2741 patients included in the analysis, 32.9% patients were on statin therapy within 90 days of ERCP.Statin therapy group had higher prevalence of CAD (44.6%,versus 23.5%,p< 0.05), hypertension (71.3%,versus 46.6%,p< 0.05) and diabetes (46.3%, versus 19.3%, p< 0.05). BMI was similar in both groups.The incidence of PEP was 7.8% in non-statin users and 6.3% in Statin users. The Chi square test indicated no statistically significant association between the both groups( p=.154).Hospital length of stay was longer in the statin therapy group(4.2+/-6.3 versus 2.8+/- 4.3,p< .05).However, the procedure time was similar in both groups ( 64.9+/-21.7 versus 66.9+/-26.7 minutes, p=0.06). Secondary outcomes of interest were also explored. 30-day admission rates were higher in the statin therapy group (17.7% versus 12.3%, p< 0.05). 30-day mortality was similar in both groups ( 1.2% vs 0.8%, p=0.03). Of note, individuals with history of deep vein thrombosis were noted to have higher Odds ( p value .000, odds ratio 2.866) of developing PEP compared to other risk factors.
Discussion: Some studies have suggested that statins could reduce the incidence and severity of PEP, yet the evidence remains inconclusive. Our study did not demonstrate any significant association between Statin use and reduced risk of PEP. However,as a retrospective analysis, this study relied on accurate documentation of statin use and the diagnosis of PEP, which may introduce information bias. Given the potential benefits, low cost, and safety profile of Statins, further prospective randomized controlled trials are warranted to explore this association more definitively.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sohaib Shabih, MD1, Daebin Im, MD, MPH1, Subash Ghimire, MD1, Amlish Gondal, MD1, Rasmita Budhathoki, MD1, Tsu Jung Yang, MD1, Madeline Mylod, MS2, Vivian Deng, MS2, Noah West, MS2, Conor Banta, 3, Michael Georgetson, MD1, Thomas McDonald, MD1. P2751 - Role of Statins in Preventing Post ERCP Pancreatitis: Insights From a Retrospective Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Guthrie Robert Packer Hospital, Sayre, PA; 2Lake Erie College of Osteopathic Medicine, Sayre, PA; 3Geisinger Commonwealth School of Medicine, Sayre, PA
Introduction: Post Endoscopic Retrograde Cholangiopancreatography (ERCP) pancreatitis (PEP) remains a significant post procedural complication. Statins have been thought to possess anti-inflammatory properties that may reduce the incidence of PEP. However, the role of Statins to prevent this event remains an area of interest.
Methods: We performed a single center retrospective comparison of patients undergoing ERCP who had active statin prescription within 90 days of the procedure versus those who were not on statins within this time frame. Variables were analyzed using Chi square test and association of comorbid conditions were calculated through binomial logarithmic regression model using SPSS v.26
Results: Out of 2741 patients included in the analysis, 32.9% patients were on statin therapy within 90 days of ERCP.Statin therapy group had higher prevalence of CAD (44.6%,versus 23.5%,p< 0.05), hypertension (71.3%,versus 46.6%,p< 0.05) and diabetes (46.3%, versus 19.3%, p< 0.05). BMI was similar in both groups.The incidence of PEP was 7.8% in non-statin users and 6.3% in Statin users. The Chi square test indicated no statistically significant association between the both groups( p=.154).Hospital length of stay was longer in the statin therapy group(4.2+/-6.3 versus 2.8+/- 4.3,p< .05).However, the procedure time was similar in both groups ( 64.9+/-21.7 versus 66.9+/-26.7 minutes, p=0.06). Secondary outcomes of interest were also explored. 30-day admission rates were higher in the statin therapy group (17.7% versus 12.3%, p< 0.05). 30-day mortality was similar in both groups ( 1.2% vs 0.8%, p=0.03). Of note, individuals with history of deep vein thrombosis were noted to have higher Odds ( p value .000, odds ratio 2.866) of developing PEP compared to other risk factors.
Discussion: Some studies have suggested that statins could reduce the incidence and severity of PEP, yet the evidence remains inconclusive. Our study did not demonstrate any significant association between Statin use and reduced risk of PEP. However,as a retrospective analysis, this study relied on accurate documentation of statin use and the diagnosis of PEP, which may introduce information bias. Given the potential benefits, low cost, and safety profile of Statins, further prospective randomized controlled trials are warranted to explore this association more definitively.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sohaib Shabih indicated no relevant financial relationships.
Daebin Im indicated no relevant financial relationships.
Subash Ghimire indicated no relevant financial relationships.
Amlish Gondal indicated no relevant financial relationships.
Rasmita Budhathoki indicated no relevant financial relationships.
Tsu Jung Yang indicated no relevant financial relationships.
Madeline Mylod indicated no relevant financial relationships.
Vivian Deng indicated no relevant financial relationships.
Noah West indicated no relevant financial relationships.
Conor Banta indicated no relevant financial relationships.
Michael Georgetson indicated no relevant financial relationships.
Thomas McDonald indicated no relevant financial relationships.
Sohaib Shabih, MD1, Daebin Im, MD, MPH1, Subash Ghimire, MD1, Amlish Gondal, MD1, Rasmita Budhathoki, MD1, Tsu Jung Yang, MD1, Madeline Mylod, MS2, Vivian Deng, MS2, Noah West, MS2, Conor Banta, 3, Michael Georgetson, MD1, Thomas McDonald, MD1. P2751 - Role of Statins in Preventing Post ERCP Pancreatitis: Insights From a Retrospective Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
