Monday Poster Session
Category: Interventional Endoscopy
P2753 - Endoscopic Transpapillary Gallbladder Stenting vs Percutaneous Cholecystostomy Tube Placement for Acute Cholecystitis in Deferred Surgery
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Daryl Ramai, MD, MPH, Msc
University of Utah Health
Salt Lake City, UT
Presenting Author(s)
Daryl Ramai, MD, MPH, Msc1, Chun-Wei Pan, MD2, Yichen Wang, MD3, Yuting Huang, MD4, John D. Morris, MD1
1University of Utah Health, Salt Lake City, UT; 2John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 3Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA; 4Mayo Clinic, Jacksonville, FL
Introduction: Laparoscopic cholecystectomy is the standard treatment for acute cholecystitis (AC), but it may not be suitable for all patients. For those who cannot undergo surgery, the conventional nonoperative intervention is a percutaneous cholecystostomy tube (PCT). However, PCT is associated with high adverse event rates, the need for scheduled reintervention, inadvertent dislodgement, and patient dissatisfaction. As an alternative, endoscopic transpapillary gallbladder drainage (ETGS) has been proposed. However, there is scare comparative data on these two approaches. We aim to assess 30-day readmission rates, adverse events, and mortality rates in these two cohorts.
Methods: We conducted a retrospective cohort study using data from the Nationwide Readmissions Database (NRD) from 2016 to 2019. We identified patients with acute cholecystitis during the index admission who underwent either ETGS or PCT using ICD-10-CM and ICD-10-PCS codes.
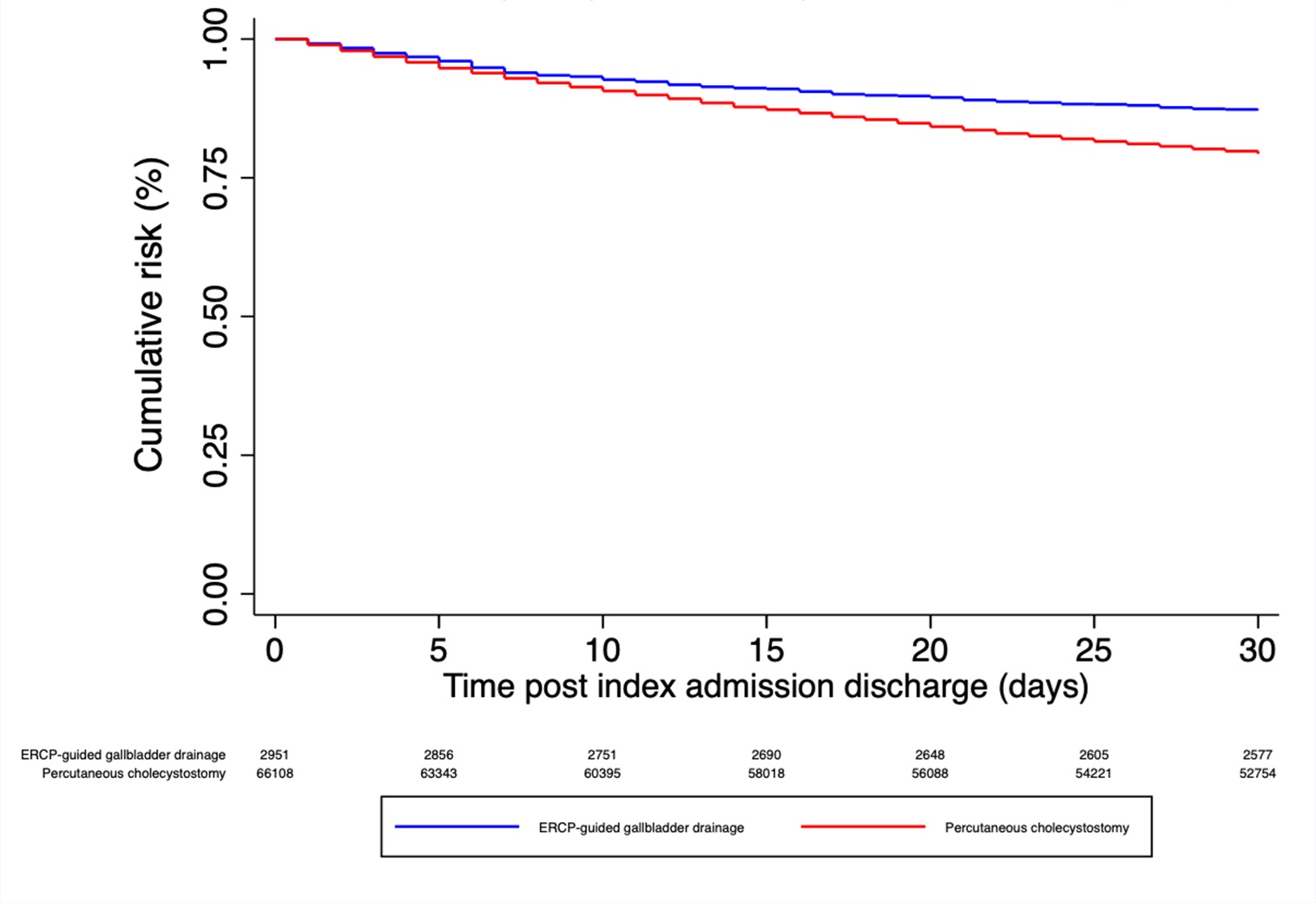
Results: During the study period, 3,592 patients (average age 63.0 years; 95% CI 62.1 – 64.0) underwent ETGS, while 80,372 patients (average 70.8 years; 95% CI 70.8 – 71.2) underwent PCT. Utilizing adjusted multivariate Cox regression analysis, compared to ETGS, PCT had a higher risk for 30-day readmission (aHR 1.47; 95% CI 1.27 to 1.71; P< 0.001). The PCT group had a significantly higher rate of readmission for acute cholecystitis compared to the ETGS group (2.72% vs 0.86%; P< 0.005). Cox proportional hazard ratio showed a 3.41-fold increased risk (95% CI: 1.99 to 5.84) for readmission in the PCT group. ETGS was consistently associated with lower rates of post-procedural adverse events compared to PCT including acute hypoxemic respiratory failure (6.69% vs. 18.48%; p< 0.001), acute renal failure (18.22% vs. 40.91%; p< 0.001), shock (0.47% vs. 1.15%; p< 0.001), and need for blood transfusions (3.27% vs. 8.13%; p< 0.001), vasopressors (1.25% vs. 4.08%; p< 0.001), and mechanical ventilation (1.25% vs. 4.08%; p< 0.001).
Discussion: In a nationwide study, we compared the outcomes of ETGS and PCT in patients who were deferred surgery. Our analysis revealed that endoscopic drainage was linked to significantly lower 30-day readmission rates, adverse events, and mortality. These findings suggest that endoscopy should be considered as the primary therapeutic approach for treating patients with acute cholecystitis when deemed unfit for surgery.
Disclosures:
Daryl Ramai, MD, MPH, Msc1, Chun-Wei Pan, MD2, Yichen Wang, MD3, Yuting Huang, MD4, John D. Morris, MD1. P2753 - Endoscopic Transpapillary Gallbladder Stenting vs Percutaneous Cholecystostomy Tube Placement for Acute Cholecystitis in Deferred Surgery, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Utah Health, Salt Lake City, UT; 2John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 3Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA; 4Mayo Clinic, Jacksonville, FL
Introduction: Laparoscopic cholecystectomy is the standard treatment for acute cholecystitis (AC), but it may not be suitable for all patients. For those who cannot undergo surgery, the conventional nonoperative intervention is a percutaneous cholecystostomy tube (PCT). However, PCT is associated with high adverse event rates, the need for scheduled reintervention, inadvertent dislodgement, and patient dissatisfaction. As an alternative, endoscopic transpapillary gallbladder drainage (ETGS) has been proposed. However, there is scare comparative data on these two approaches. We aim to assess 30-day readmission rates, adverse events, and mortality rates in these two cohorts.
Methods: We conducted a retrospective cohort study using data from the Nationwide Readmissions Database (NRD) from 2016 to 2019. We identified patients with acute cholecystitis during the index admission who underwent either ETGS or PCT using ICD-10-CM and ICD-10-PCS codes.
Results: During the study period, 3,592 patients (average age 63.0 years; 95% CI 62.1 – 64.0) underwent ETGS, while 80,372 patients (average 70.8 years; 95% CI 70.8 – 71.2) underwent PCT. Utilizing adjusted multivariate Cox regression analysis, compared to ETGS, PCT had a higher risk for 30-day readmission (aHR 1.47; 95% CI 1.27 to 1.71; P< 0.001). The PCT group had a significantly higher rate of readmission for acute cholecystitis compared to the ETGS group (2.72% vs 0.86%; P< 0.005). Cox proportional hazard ratio showed a 3.41-fold increased risk (95% CI: 1.99 to 5.84) for readmission in the PCT group. ETGS was consistently associated with lower rates of post-procedural adverse events compared to PCT including acute hypoxemic respiratory failure (6.69% vs. 18.48%; p< 0.001), acute renal failure (18.22% vs. 40.91%; p< 0.001), shock (0.47% vs. 1.15%; p< 0.001), and need for blood transfusions (3.27% vs. 8.13%; p< 0.001), vasopressors (1.25% vs. 4.08%; p< 0.001), and mechanical ventilation (1.25% vs. 4.08%; p< 0.001).
Discussion: In a nationwide study, we compared the outcomes of ETGS and PCT in patients who were deferred surgery. Our analysis revealed that endoscopic drainage was linked to significantly lower 30-day readmission rates, adverse events, and mortality. These findings suggest that endoscopy should be considered as the primary therapeutic approach for treating patients with acute cholecystitis when deemed unfit for surgery.
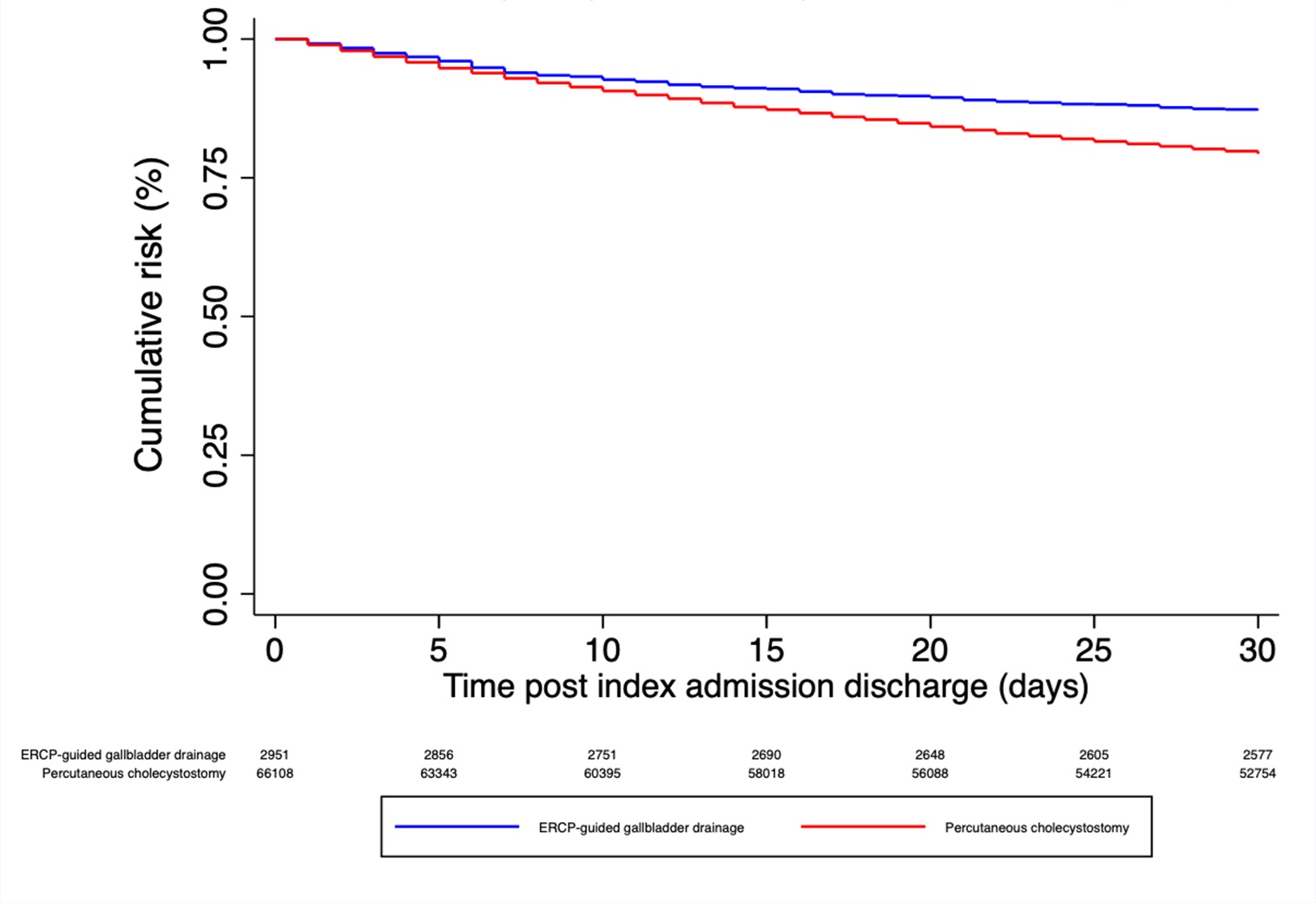
Figure: Kaplan-Meier curve of all-cause 30-day readmission comparing endoscopic transpapillary gallbladder stenting (ETGS) vs percutaneous cholecystostomy tube (PCT) placement.
Disclosures:
Daryl Ramai indicated no relevant financial relationships.
Chun-Wei Pan indicated no relevant financial relationships.
Yichen Wang indicated no relevant financial relationships.
Yuting Huang indicated no relevant financial relationships.
John Morris indicated no relevant financial relationships.
Daryl Ramai, MD, MPH, Msc1, Chun-Wei Pan, MD2, Yichen Wang, MD3, Yuting Huang, MD4, John D. Morris, MD1. P2753 - Endoscopic Transpapillary Gallbladder Stenting vs Percutaneous Cholecystostomy Tube Placement for Acute Cholecystitis in Deferred Surgery, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
