Monday Poster Session
Category: Interventional Endoscopy
P2757 - Outcomes of Endoscopic Full-Thickness Resection vs Submucosal Tunneling Endoscopic Resection of Gastric Gastrointestinal Stromal Tumors: A Systematic Review and Meta-Analysis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Shravya Ginnaram, MD
Jefferson Abington Hospital
Willow Grove, PA
Presenting Author(s)
Shravya Ginnaram, MD1, Pradeep Yarra, MD2, Dawood Tahir, MD1, Wissam Kiwan, MD3, Antonio R. Cheesman, MD4, Marina Kim, MD4
1Jefferson Abington Hospital, Willow Grove, PA; 2Saint Louis University School of Medicine, St. Louis, MO; 3Saint Louis University, St. Louis, MO; 4SSM Health Saint Louis University Hospital, St. Louis, MO
Introduction: Gastric subepithelial tumors such as gastrointestinal stromal tumors (GISTs) are predominantly benign but carry the risk of malignancy, necessitating precise and safe resection techniques. ESGE suggests considering endoscopic removal of histologically proven gastric GISTs < 20 mm as an alternative to surveillance. Endoscopic submucosal dissection (ESD) carries risks of full-thickness perforation due to the common origin from the muscularis propria, leading to the development of techniques like endoscopic full-thickness resection (EFTR) and submucosal tunneling endoscopic resection (STER). As there is no consensus on the optimal resection technique for gastric GISTs, this study aims to evaluate the outcomes of EFTR compared to STER.
Methods: We conducted a systematic review and meta-analysis per PRISMA guidelines. Five studies were selected from MEDLINE/PubMed, OVID and Cochrane Central Register of Controlled Trials, comparing EFTR and STER across four key outcomes: en-bloc resection rate, length of stay (LOS), combined adverse event rates (fever > 38 °C, acute or delayed major bleeding, abdominal pain, peritonitis, and mucosal injury), and tumor recurrence rate. The analysis included a total sample size of 149 patients for EFTR and 66 for STER.
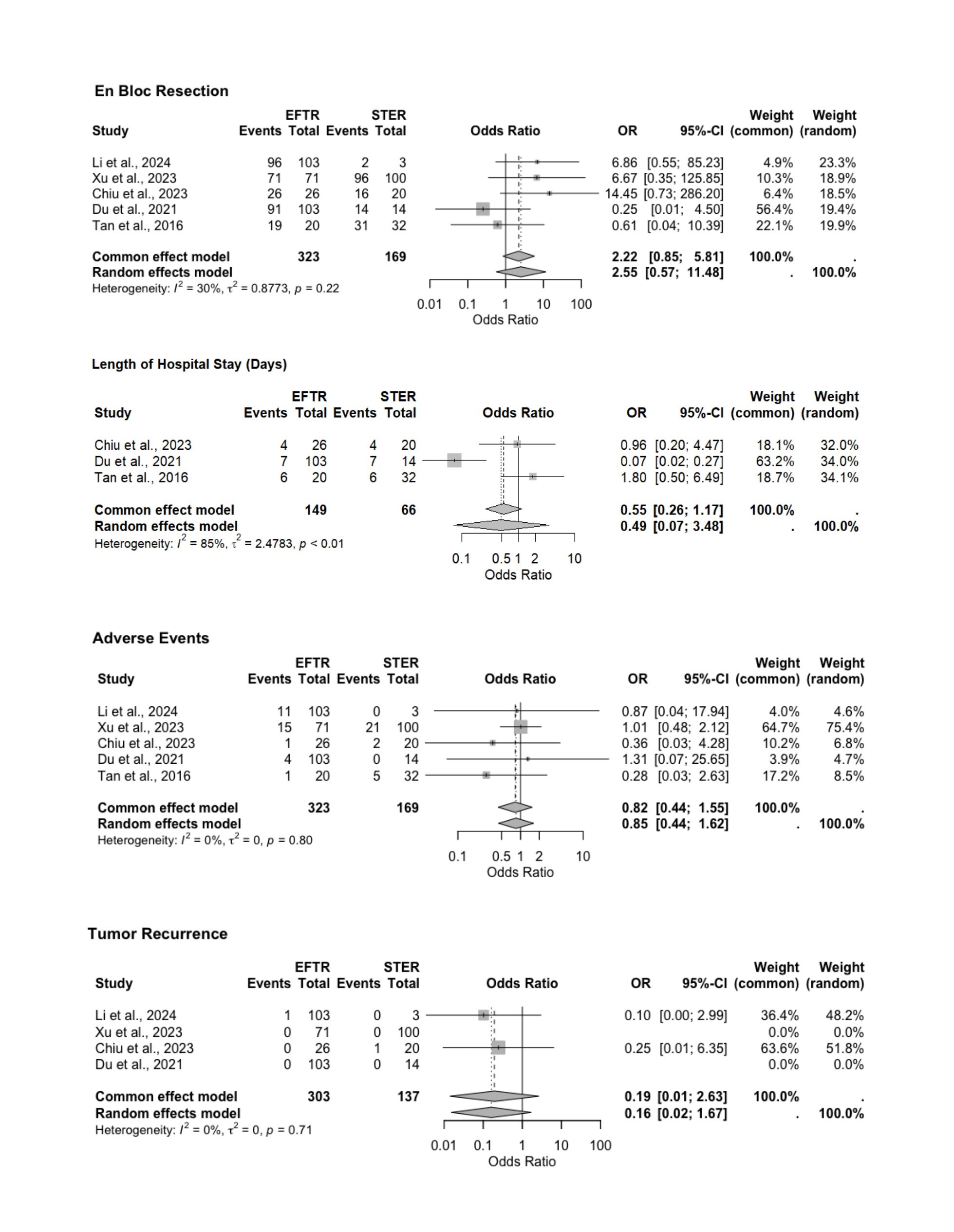
Results: The mean lesion size for EFTR was 17 mm ± 4.8 mm and 19.3 mm ± 2.7 mm for STER. EFTR showed a superior en-bloc resection rate (OR = 2.55, 95% CI [0.57; 11.48]), but this was not statistically significant. Despite high heterogeneity in LOS data (I² = 85%), there was no preference for either procedure (OR = 0.49, 95% CI [0.07; 3.48]). Adverse event rates were low across both, though marginally lower in EFTR (OR = 0.85, 95% CI [0.44; 1.62]). Tumor recurrence rates were low for both (OR = 0.16, 95% CI [0.02; 1.67]) but not statistically significant.
Discussion: EFTR and STER are viable therapeutic options for gastric GISTs. Statistically significant differences were not found in the measured outcomes. However, EFTR may provide better outcomes in achieving complete tumor resection and reducing adverse events, while STER offers advantages in reducing LOS. Both treatments reduce tumor recurrence, indicating efficacy in long-term management of gastric GISTs. Clinical decisions should balance these findings with patient-specific factors like average lesion size and procedural expertise to optimize outcomes. Future studies should focus on larger, diverse populations using standardized protocols and RCTs to improve validity and extend these findings.
Disclosures:
Shravya Ginnaram, MD1, Pradeep Yarra, MD2, Dawood Tahir, MD1, Wissam Kiwan, MD3, Antonio R. Cheesman, MD4, Marina Kim, MD4. P2757 - Outcomes of Endoscopic Full-Thickness Resection vs Submucosal Tunneling Endoscopic Resection of Gastric Gastrointestinal Stromal Tumors: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Jefferson Abington Hospital, Willow Grove, PA; 2Saint Louis University School of Medicine, St. Louis, MO; 3Saint Louis University, St. Louis, MO; 4SSM Health Saint Louis University Hospital, St. Louis, MO
Introduction: Gastric subepithelial tumors such as gastrointestinal stromal tumors (GISTs) are predominantly benign but carry the risk of malignancy, necessitating precise and safe resection techniques. ESGE suggests considering endoscopic removal of histologically proven gastric GISTs < 20 mm as an alternative to surveillance. Endoscopic submucosal dissection (ESD) carries risks of full-thickness perforation due to the common origin from the muscularis propria, leading to the development of techniques like endoscopic full-thickness resection (EFTR) and submucosal tunneling endoscopic resection (STER). As there is no consensus on the optimal resection technique for gastric GISTs, this study aims to evaluate the outcomes of EFTR compared to STER.
Methods: We conducted a systematic review and meta-analysis per PRISMA guidelines. Five studies were selected from MEDLINE/PubMed, OVID and Cochrane Central Register of Controlled Trials, comparing EFTR and STER across four key outcomes: en-bloc resection rate, length of stay (LOS), combined adverse event rates (fever > 38 °C, acute or delayed major bleeding, abdominal pain, peritonitis, and mucosal injury), and tumor recurrence rate. The analysis included a total sample size of 149 patients for EFTR and 66 for STER.
Results: The mean lesion size for EFTR was 17 mm ± 4.8 mm and 19.3 mm ± 2.7 mm for STER. EFTR showed a superior en-bloc resection rate (OR = 2.55, 95% CI [0.57; 11.48]), but this was not statistically significant. Despite high heterogeneity in LOS data (I² = 85%), there was no preference for either procedure (OR = 0.49, 95% CI [0.07; 3.48]). Adverse event rates were low across both, though marginally lower in EFTR (OR = 0.85, 95% CI [0.44; 1.62]). Tumor recurrence rates were low for both (OR = 0.16, 95% CI [0.02; 1.67]) but not statistically significant.
Discussion: EFTR and STER are viable therapeutic options for gastric GISTs. Statistically significant differences were not found in the measured outcomes. However, EFTR may provide better outcomes in achieving complete tumor resection and reducing adverse events, while STER offers advantages in reducing LOS. Both treatments reduce tumor recurrence, indicating efficacy in long-term management of gastric GISTs. Clinical decisions should balance these findings with patient-specific factors like average lesion size and procedural expertise to optimize outcomes. Future studies should focus on larger, diverse populations using standardized protocols and RCTs to improve validity and extend these findings.
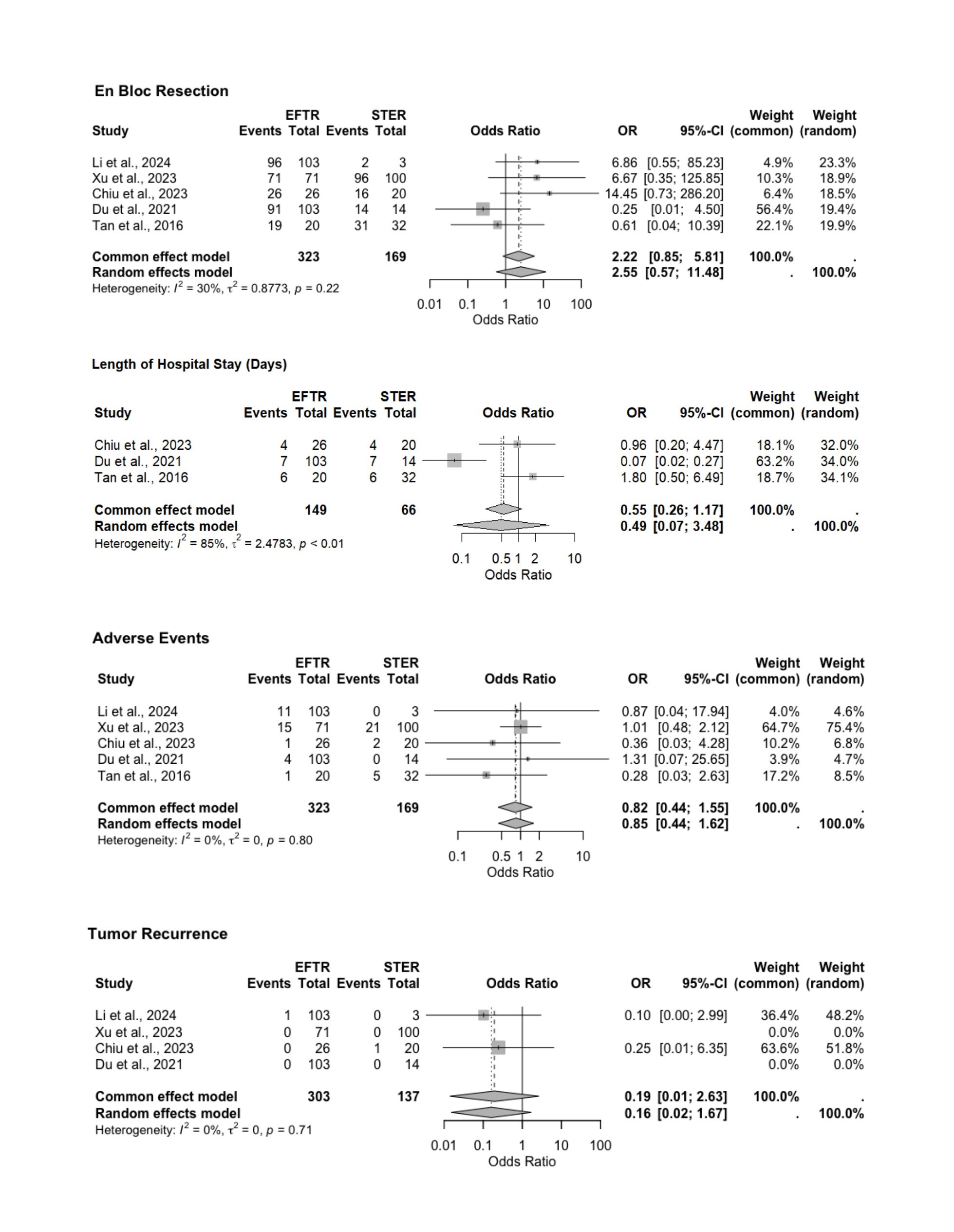
Figure: Forest Plot of Studies Comparing Outcomes for Endoscopic Full Thickness Resection (EFTR) versus Submucosal Tunneling Endoscopic Resection (STER)
Disclosures:
Shravya Ginnaram indicated no relevant financial relationships.
Pradeep Yarra indicated no relevant financial relationships.
Dawood Tahir indicated no relevant financial relationships.
Wissam Kiwan indicated no relevant financial relationships.
Antonio Cheesman indicated no relevant financial relationships.
Marina Kim indicated no relevant financial relationships.
Shravya Ginnaram, MD1, Pradeep Yarra, MD2, Dawood Tahir, MD1, Wissam Kiwan, MD3, Antonio R. Cheesman, MD4, Marina Kim, MD4. P2757 - Outcomes of Endoscopic Full-Thickness Resection vs Submucosal Tunneling Endoscopic Resection of Gastric Gastrointestinal Stromal Tumors: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
