Monday Poster Session
Category: Interventional Endoscopy
P2789 - Endoscopic Ultrasound Functionality for a Standard Upper Endoscope: Initial U.S. Experience
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Seth A. Gross, MD, FACG
Associate Professor of Medicine, NYU School of Medicine; Chief of Gastroenterology, Tisch Hospital
NYU Langone Health
New York, NY
Presenting Author(s)
Award: ACG Outstanding Research Award in the Interventional Endoscopy Category
Award: Presidential Poster Award
Seth Gross, MD1, Rebecca I. Siegel, 1, Stuart Akerman, MD2, Isaac Raijman, MD3, Ruel Garcia, MD4, Marco Paez, MD5, Brian Lim, MD6
1NYU Langone Health, New York, NY; 2Digestive Health Associates of Texas, Dallas, TX; 3Texas Digestive Disease Consultants, Houston, TX; 4Genesis Healthcare, Los Gatos, CA; 5United Medical Doctors, Riverside, CA; 6United Medical Doctors, Irvine, CA
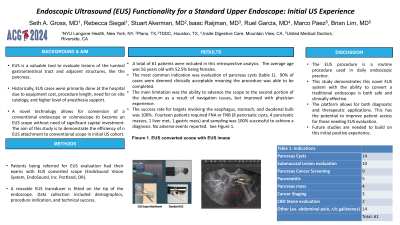
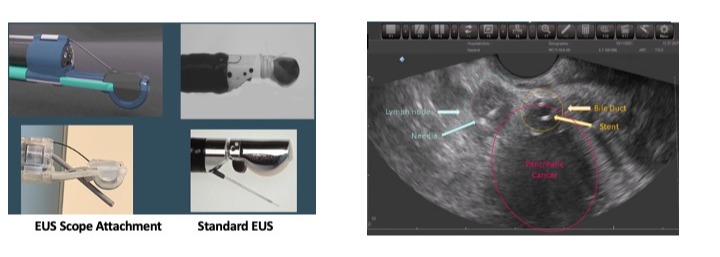
Introduction: Endoscopic ultrasound (EUS) is a valuable tool to evaluate lesions of the luminal gastrointestinal tract and adjacent structures, like the pancreas. Historically, EUS cases were primarily done at the hospital due to equipment cost, procedure length, need for on-site cytology, and higher level of anesthesia support. However, improvement in tissue acquisition with core biopsy needles eliminating need for on-site cytology, decrease case length, and monitored anesthesia care allows EUS to be preformed outside the hospital, such as ambulatory care center (ASC). A novel technology allows for conversion of a conventional endoscope or colonoscope to become an EUS scope without need of significant capital investment. The aim of this study is to demonstrate the efficiency of n EUS attachment to conventional scope in initial US cohort.
Methods: Patients being referred for EUS evaluation had their exams with EUS converted scope (EndoSound Vision Systems, EndoSound, Inc. Portland, OR). A reusable EUS transducer is fitted on the tip of the endoscope. Data collection included demographics, procedure indication, and technical success.
Results: A total of 61 patients were included in this retrospective analysis. The average age was 56 years old with 52.5% being females. The most common indication was evaluation of pancreas cysts (table 1). 90% of cased were deemed clinically acceptable meaning the procedure was able to be fully completed. The main limitation was the ability to advance the scope to the second portion of the duodenum as a result of navigation issues. this improved with Physcian experience. The success rate for targets involving the esophagus, stomach, duodenal bulb were 100%. Fourteen patients required FNA or FNB ( 8 pancreatic cysts, 4 pancreatic masses, 1 liver metastasis, 1 gastric was) and sampling was 100% successful to achieve a diagnosis. No adverse events reported. See figure 1.
Discussion: The EUS procedure is a routine procedure used in daily clinical practice, mainly at a hospital. This study demonstrates this novel EUS system with the ability to convert a traditional endoscope is both safe and clinically effective. The platform allows for both diagnostic and therapeutic applications. This has the potential to improve patient access for those needing EUS evaluation. Further studies are needed to build on this initial positive experience.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Seth Gross, MD1, Rebecca I. Siegel, 1, Stuart Akerman, MD2, Isaac Raijman, MD3, Ruel Garcia, MD4, Marco Paez, MD5, Brian Lim, MD6. P2789 - Endoscopic Ultrasound Functionality for a Standard Upper Endoscope: Initial U.S. Experience, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Award: Presidential Poster Award
Seth Gross, MD1, Rebecca I. Siegel, 1, Stuart Akerman, MD2, Isaac Raijman, MD3, Ruel Garcia, MD4, Marco Paez, MD5, Brian Lim, MD6
1NYU Langone Health, New York, NY; 2Digestive Health Associates of Texas, Dallas, TX; 3Texas Digestive Disease Consultants, Houston, TX; 4Genesis Healthcare, Los Gatos, CA; 5United Medical Doctors, Riverside, CA; 6United Medical Doctors, Irvine, CA
Introduction: Endoscopic ultrasound (EUS) is a valuable tool to evaluate lesions of the luminal gastrointestinal tract and adjacent structures, like the pancreas. Historically, EUS cases were primarily done at the hospital due to equipment cost, procedure length, need for on-site cytology, and higher level of anesthesia support. However, improvement in tissue acquisition with core biopsy needles eliminating need for on-site cytology, decrease case length, and monitored anesthesia care allows EUS to be preformed outside the hospital, such as ambulatory care center (ASC). A novel technology allows for conversion of a conventional endoscope or colonoscope to become an EUS scope without need of significant capital investment. The aim of this study is to demonstrate the efficiency of n EUS attachment to conventional scope in initial US cohort.
Methods: Patients being referred for EUS evaluation had their exams with EUS converted scope (EndoSound Vision Systems, EndoSound, Inc. Portland, OR). A reusable EUS transducer is fitted on the tip of the endoscope. Data collection included demographics, procedure indication, and technical success.
Results: A total of 61 patients were included in this retrospective analysis. The average age was 56 years old with 52.5% being females. The most common indication was evaluation of pancreas cysts (table 1). 90% of cased were deemed clinically acceptable meaning the procedure was able to be fully completed. The main limitation was the ability to advance the scope to the second portion of the duodenum as a result of navigation issues. this improved with Physcian experience. The success rate for targets involving the esophagus, stomach, duodenal bulb were 100%. Fourteen patients required FNA or FNB ( 8 pancreatic cysts, 4 pancreatic masses, 1 liver metastasis, 1 gastric was) and sampling was 100% successful to achieve a diagnosis. No adverse events reported. See figure 1.
Discussion: The EUS procedure is a routine procedure used in daily clinical practice, mainly at a hospital. This study demonstrates this novel EUS system with the ability to convert a traditional endoscope is both safe and clinically effective. The platform allows for both diagnostic and therapeutic applications. This has the potential to improve patient access for those needing EUS evaluation. Further studies are needed to build on this initial positive experience.
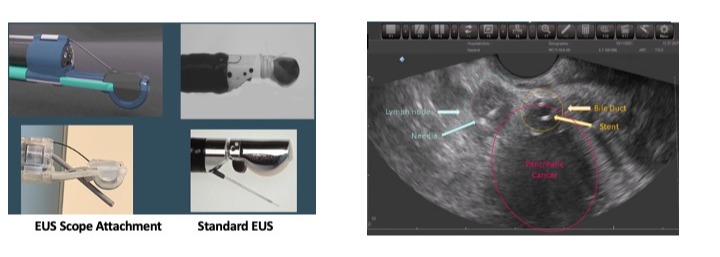
Figure: Figure 1: EUS attachment versus standard EUS. EUS attachment demonstrating pancreas mass.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Seth Gross: Cook – Consultant. Medtronic – Consultant. Microtech – Consultant. Olympis – Consultant. Provation – Consultant.
Rebecca Siegel indicated no relevant financial relationships.
Stuart Akerman: EndoSound – Advisor or Review Panel Member. Nestle Health – Speakers Bureau.
Isaac Raijman: Endosound – Advisory Committee/Board Member.
Ruel Garcia indicated no relevant financial relationships.
Marco Paez indicated no relevant financial relationships.
Brian Lim indicated no relevant financial relationships.
Seth Gross, MD1, Rebecca I. Siegel, 1, Stuart Akerman, MD2, Isaac Raijman, MD3, Ruel Garcia, MD4, Marco Paez, MD5, Brian Lim, MD6. P2789 - Endoscopic Ultrasound Functionality for a Standard Upper Endoscope: Initial U.S. Experience, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

