Monday Poster Session
Category: Interventional Endoscopy
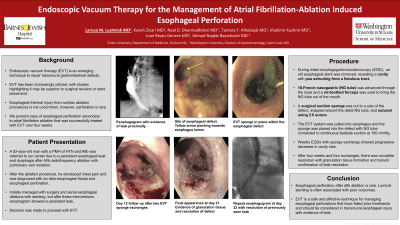
P2811 - Endoscopic Vacuum Therapy for the Management of Atrial Fibrillation-Induced Esophageal Perforation
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Larissa M. Lushniak, MD
Washington University School of Medicine in St. Louis
Durham, NC
Presenting Author(s)
Larissa Lushniak, MD1, Kaveh Zivari, MD1, Neal Dharmadhikari, MD1, Vladimir Kushnir, MD1, Juan Reyes Genere, MD1, Ahmad Najdat Bazarbashi, MD2
1Washington University School of Medicine in St. Louis, St. Louis, MO; 2Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, MO
Introduction: Endoscopic vacuum therapy (EVT) is an emerging technique to repair transmural gastrointestinal defects. EVT has been increasingly utilized with studies highlighting it may be superior to surgical revision or stent placement. Esophageal thermal injury from atrial fibrillation (AF) ablation is not uncommon, however full thickness perforation is rare. We present a case of esophageal perforation secondary to atrial fibrillation radiofrequency ablation that was successfully treated with EVT.
Case Description/Methods: A 52-year-old man presented with persistent esophageal defect caused by AF ablation with pulmonary vein isolation. Four months prior, the patient developed chest pain after the ablation procedure and was found to have an atrio-esophageal fistula and esophageal tracheobronchial perforation. He was managed with surgical repair of the fistula and left atrial perforation, bronchial stenting, J-tube placement and serial esophageal stent placement. Despite this, an esophagogram showed a persistent leak. The patient was referred to our center for management of the leak with EVT.
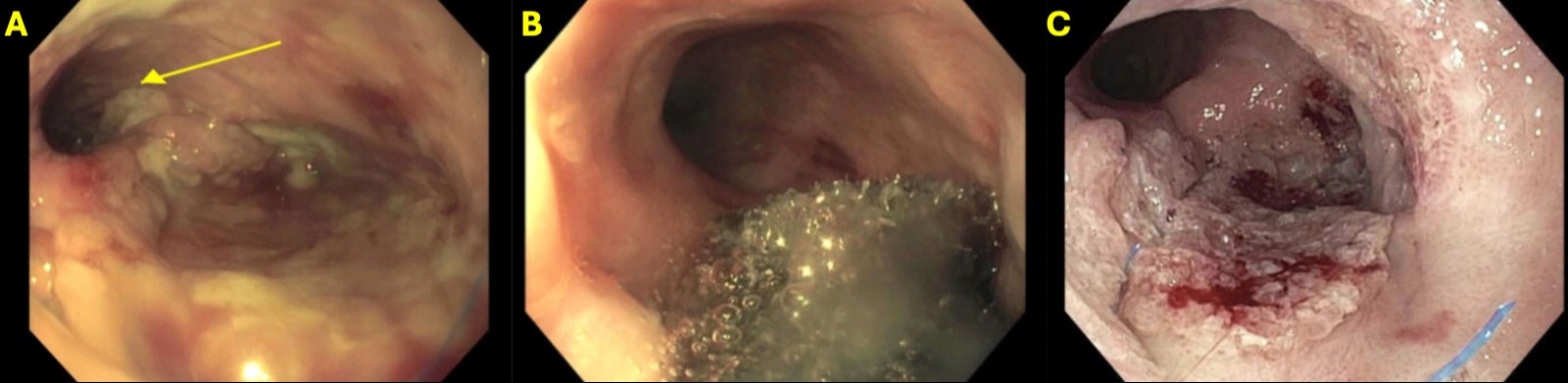
During a repeat EGD, a previously placed esophageal stent was removed to reveal a cavity with pus extruding consistent with an esophageal defect (image 1A). A 16F nasogastric (NG) tube was advanced through the nose into the oropharynx and was brought out through the mouth using rat-toothed forceps. Surgical black suction sponge was cut to an approximate size of the visualized defect. The distal NG tube was wrapped with this sponge which was sutured down using 2.0 suture. The wound vac system was pulled down the esophagus and the sponge was placed into the esophageal defect (Image 1B). The NG tube was connected to a continuous bedside suction at 100 mmHg while the patient was kept NPO with J-tube feeding.
Three subsequent serial EGDs with sponge exchange over the next three weeks (one exchange per week) showed marked decrease in the size of the cavity. The fourth and final EGD showed continued reduction and near complete resolution of initial esophageal defect and granulation tissue formation consistent with a healed defect (image 1C). A final esophagogram showed complete resolution of the leak. At a six-month follow-up visit, the patient was tolerating oral intake without symptoms.
Discussion: This case highlights the successful and safe management of an esophageal transmural defect with EVT after a rare complication from cardiovascular ablative therapy.
Disclosures:
Larissa Lushniak, MD1, Kaveh Zivari, MD1, Neal Dharmadhikari, MD1, Vladimir Kushnir, MD1, Juan Reyes Genere, MD1, Ahmad Najdat Bazarbashi, MD2. P2811 - Endoscopic Vacuum Therapy for the Management of Atrial Fibrillation-Induced Esophageal Perforation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Washington University School of Medicine in St. Louis, St. Louis, MO; 2Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, MO
Introduction: Endoscopic vacuum therapy (EVT) is an emerging technique to repair transmural gastrointestinal defects. EVT has been increasingly utilized with studies highlighting it may be superior to surgical revision or stent placement. Esophageal thermal injury from atrial fibrillation (AF) ablation is not uncommon, however full thickness perforation is rare. We present a case of esophageal perforation secondary to atrial fibrillation radiofrequency ablation that was successfully treated with EVT.
Case Description/Methods: A 52-year-old man presented with persistent esophageal defect caused by AF ablation with pulmonary vein isolation. Four months prior, the patient developed chest pain after the ablation procedure and was found to have an atrio-esophageal fistula and esophageal tracheobronchial perforation. He was managed with surgical repair of the fistula and left atrial perforation, bronchial stenting, J-tube placement and serial esophageal stent placement. Despite this, an esophagogram showed a persistent leak. The patient was referred to our center for management of the leak with EVT.
During a repeat EGD, a previously placed esophageal stent was removed to reveal a cavity with pus extruding consistent with an esophageal defect (image 1A). A 16F nasogastric (NG) tube was advanced through the nose into the oropharynx and was brought out through the mouth using rat-toothed forceps. Surgical black suction sponge was cut to an approximate size of the visualized defect. The distal NG tube was wrapped with this sponge which was sutured down using 2.0 suture. The wound vac system was pulled down the esophagus and the sponge was placed into the esophageal defect (Image 1B). The NG tube was connected to a continuous bedside suction at 100 mmHg while the patient was kept NPO with J-tube feeding.
Three subsequent serial EGDs with sponge exchange over the next three weeks (one exchange per week) showed marked decrease in the size of the cavity. The fourth and final EGD showed continued reduction and near complete resolution of initial esophageal defect and granulation tissue formation consistent with a healed defect (image 1C). A final esophagogram showed complete resolution of the leak. At a six-month follow-up visit, the patient was tolerating oral intake without symptoms.
Discussion: This case highlights the successful and safe management of an esophageal transmural defect with EVT after a rare complication from cardiovascular ablative therapy.
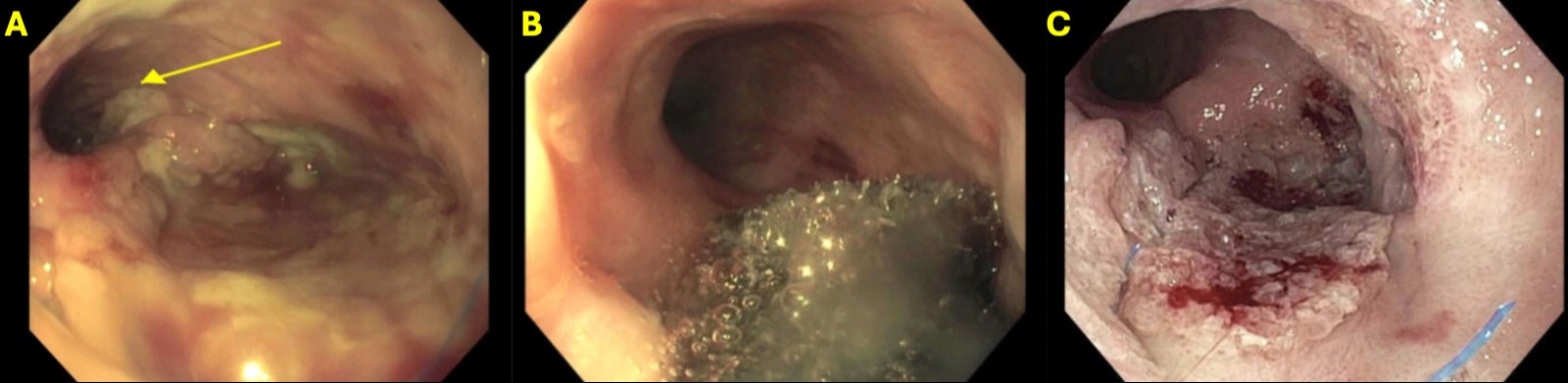
Figure: A) Esophageal defect with pus emanating. Yellow arrow pointing at esophagus lumen.
B) Initial EVT placement in esophageal defect
C) Granulation tissue formation consistent with a healed defect
B) Initial EVT placement in esophageal defect
C) Granulation tissue formation consistent with a healed defect
Disclosures:
Larissa Lushniak indicated no relevant financial relationships.
Kaveh Zivari indicated no relevant financial relationships.
Neal Dharmadhikari indicated no relevant financial relationships.
Vladimir Kushnir indicated no relevant financial relationships.
Juan Reyes Genere: Boston Scientific – Consultant. Edulis Therapuetics – Consultant.
Ahmad Najdat Bazarbashi indicated no relevant financial relationships.
Larissa Lushniak, MD1, Kaveh Zivari, MD1, Neal Dharmadhikari, MD1, Vladimir Kushnir, MD1, Juan Reyes Genere, MD1, Ahmad Najdat Bazarbashi, MD2. P2811 - Endoscopic Vacuum Therapy for the Management of Atrial Fibrillation-Induced Esophageal Perforation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
