Monday Poster Session
Category: Interventional Endoscopy
P2820 - A Rare Case of Stent Migration and Perforation of the Opposite Wall of the Duodenum and the Adjacent Ascending Colon
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Hassan Ali Al Saleh, DO, MS
University at Buffalo
Buffalo, NY
Presenting Author(s)
Hassan Ali Al Saleh, DO, MS1, Michael j. Farrell, MD2, Matthew J. Hudson, MD2
1University at Buffalo, Buffalo, NY; 2University of Buffalo Jacobs School of Medicine, Buffalo, NY
Introduction: Endoscopic biliary stent (EBS) insertion is a well-established treatment for hepato-pancreato-biliary (HPB) disorders. While plastic stents carry a risk of migration from the bile duct into the bowel lumen and subsequent perforation across the opposite duodenal wall or distally, this is rarely reported and has been historically managed using endoclips or an over-the-scope clip (OTSC). We report a case of partial migration of a plastic EBS with perforation of both the opposite wall of the duodenum and the adjacent ascending colon, that was managed via colonoscopic removal of the stent and suturing of an entero-colonic fistula.
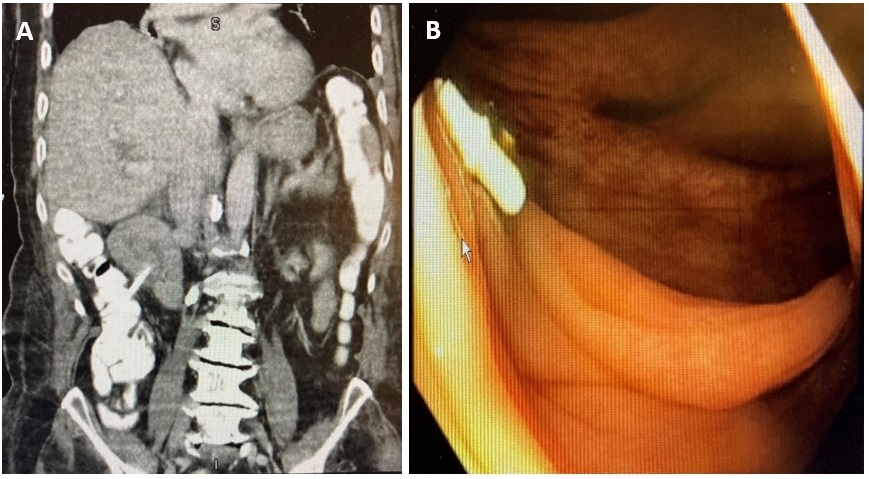
Case Description/Methods: An 85 y/o male with a history of hypertension, dementia, and choledocholithiasis previously managed via endoscopic retrograde cholangiopancreatography (ERCP) presented with right upper quadrant pain and fever. Commuted tomography (CT) of the abdomen revealed a hydropic gallbladder with wall thickening, and a stent originating from the bile duct and terminating distally across the duodenal wall and into the lumen of the ascending colon without free air (Fig. A). The patient has had a plastic stent placed into the main bile duct for choledocholithiasis 36 months prior, but had not followed up for stent removal due to the SARS-CoV-2 pandemic. Given his comorbidities, the patient was treated conservatively for acute cholecystitis, and a cholecystostomy tube was placed. Upon resolution of sepsis, colonoscopy revealed a plastic EBS had distally migrated and penetrated across the opposite wall of the duodenum and through the ascending colon, emanating from a fistula of 5-6 mm in diameter (Fig. B). The stent was removed with a snare, and the colonic aspect of the fistula was fulgurated using argon plasma coagulation, and closed using endoscopic suturing. Duodenoscopy following colonoscopy revealed closure of the fistula, and an ERCP extracted residual stone debris from the bile duct.
Discussion: While plastic EBS insertion is a widely used practice for the short-term management of biliary obstruction, stent migration is a known complication and can lead to perforations, with the duodenum being the most common site of perforation. Our case describes a unique perforation of the duodenum and the ascending colon, leading to an entero-colonic fistula. It shows that such a complication can be managed endoscopically, and highlights the importance of adequate clinical follow up after placement of EBS, as delayed follow-up likely contributed to this complication.
Disclosures:
Hassan Ali Al Saleh, DO, MS1, Michael j. Farrell, MD2, Matthew J. Hudson, MD2. P2820 - A Rare Case of Stent Migration and Perforation of the Opposite Wall of the Duodenum and the Adjacent Ascending Colon, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University at Buffalo, Buffalo, NY; 2University of Buffalo Jacobs School of Medicine, Buffalo, NY
Introduction: Endoscopic biliary stent (EBS) insertion is a well-established treatment for hepato-pancreato-biliary (HPB) disorders. While plastic stents carry a risk of migration from the bile duct into the bowel lumen and subsequent perforation across the opposite duodenal wall or distally, this is rarely reported and has been historically managed using endoclips or an over-the-scope clip (OTSC). We report a case of partial migration of a plastic EBS with perforation of both the opposite wall of the duodenum and the adjacent ascending colon, that was managed via colonoscopic removal of the stent and suturing of an entero-colonic fistula.
Case Description/Methods: An 85 y/o male with a history of hypertension, dementia, and choledocholithiasis previously managed via endoscopic retrograde cholangiopancreatography (ERCP) presented with right upper quadrant pain and fever. Commuted tomography (CT) of the abdomen revealed a hydropic gallbladder with wall thickening, and a stent originating from the bile duct and terminating distally across the duodenal wall and into the lumen of the ascending colon without free air (Fig. A). The patient has had a plastic stent placed into the main bile duct for choledocholithiasis 36 months prior, but had not followed up for stent removal due to the SARS-CoV-2 pandemic. Given his comorbidities, the patient was treated conservatively for acute cholecystitis, and a cholecystostomy tube was placed. Upon resolution of sepsis, colonoscopy revealed a plastic EBS had distally migrated and penetrated across the opposite wall of the duodenum and through the ascending colon, emanating from a fistula of 5-6 mm in diameter (Fig. B). The stent was removed with a snare, and the colonic aspect of the fistula was fulgurated using argon plasma coagulation, and closed using endoscopic suturing. Duodenoscopy following colonoscopy revealed closure of the fistula, and an ERCP extracted residual stone debris from the bile duct.
Discussion: While plastic EBS insertion is a widely used practice for the short-term management of biliary obstruction, stent migration is a known complication and can lead to perforations, with the duodenum being the most common site of perforation. Our case describes a unique perforation of the duodenum and the ascending colon, leading to an entero-colonic fistula. It shows that such a complication can be managed endoscopically, and highlights the importance of adequate clinical follow up after placement of EBS, as delayed follow-up likely contributed to this complication.
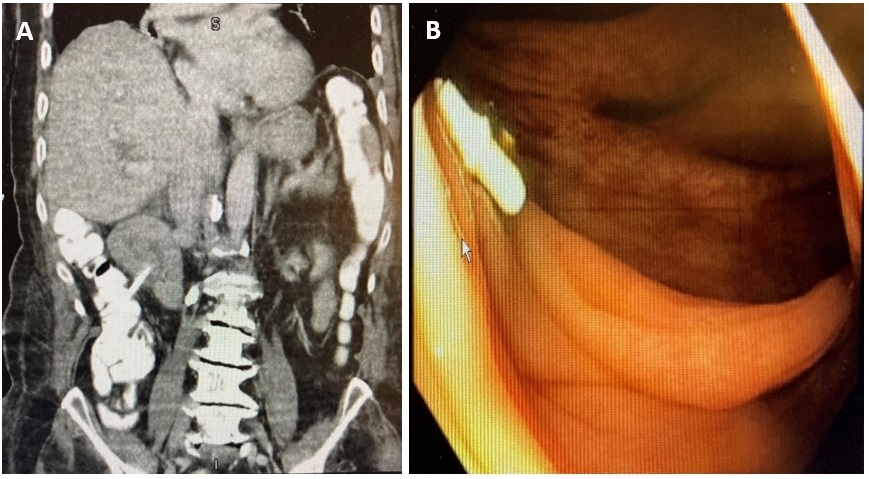
Figure: A coronal computed tomography (CT) view of the abdomen revealing a radiopaque stent originating from the bile duct and terminating distally across the duodenal wall and into the lumen of the ascending colon; no free air was noted (A). Colonoscopy revealed a plastic endoscopic biliary stent (EBS) with distal migration and penetration across the opposite wall of the duodenum and through the wall of the ascending colon, emanating from a fistula that was approximately 5-6 mm in diameter (B).
Disclosures:
Hassan Ali Al Saleh indicated no relevant financial relationships.
Michael Farrell indicated no relevant financial relationships.
Matthew Hudson indicated no relevant financial relationships.
Hassan Ali Al Saleh, DO, MS1, Michael j. Farrell, MD2, Matthew J. Hudson, MD2. P2820 - A Rare Case of Stent Migration and Perforation of the Opposite Wall of the Duodenum and the Adjacent Ascending Colon, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
