Monday Poster Session
Category: Interventional Endoscopy
P2836 - Effective Antegrade EUS-Guided Puncture With Stent Placement in Completely Obliterated Esophagus
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Nina Quirk, MS, MD
University of Texas Health, McGovern Medical School
Houston, TX
Presenting Author(s)
Nina Quirk, MS, MD, Nitish Mittal, MD, Yllen Hernandez Blanco, MD, Vaibhav Wadhwa, MD, FACG
University of Texas Health, McGovern Medical School, Houston, TX
Introduction: Complete obliterated esophagus (COE) is a consequence of advanced esophageal strictures that is challenging to treat due to technique complexity and high rate of complications. Esophageal stenting has been used in COE; however, there is currently no standard protocol or guideline for COE treatment given the technique’s difficulty and considerable risk of bleeding and perforation. In this report, we describe a unique and successful case of COE recanalization using only anterograde endoscopic ultrasound (EUS)-guided puncture technique with stent placement.
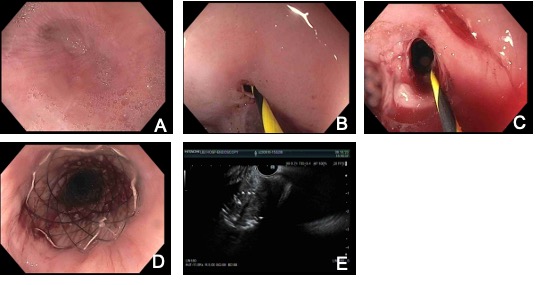
Case Description/Methods: We present a case of 67 year old male with a past medical history of necrotizing gallstone pancreatitis in 4/2017. The patient underwent endoscopic retrograde cholangiopancreatography (ERCP) with stones and sludge removal and biliary stent placement. He subsequently developed complications that lead to numerous abdominal surgeries over the course of a year. On 3/2018 due to inability to tolerate anything by mouth, he underwent esophagogastroduodenoscopy (EGD) with findings of gastro-jejunal (GJ) anastomotic stricture. Several later EGDs demonstrated recurrent esophageal strictures requiring multiple dilations. EGD on 5/2020 showed high grade long esophageal anastomotic stricture status post 7 mm CRE balloon dilation, 80mg Kenalog injection, and partially covered 18mm X 123mm esophageal stent placement under fluoroscopy guidance. He continued to suffer from dysphagia and upper GI bleeds. EGD/EUS on 8/2023 had findings of COE status post EUS-guided access to the distal esophagus with fine needle injection and fluoroscopic confirmation of position. With wire-guided dilation of the tract, placement of an esophageal stent across the proximal extent in the upper esophagus and the distal extent in the distal esophagus within the lumen of the prior stent was achieved. Barium swallow exam confirmed stent placement and no leakage. Recent EGD in 1/2024 showed esophageal stricture status post dilation to 15 mm. After the stenting in 8/2023, the patient has had remarkable clinical and nutritional improvement with resolution of his electrolyte abnormalities and anemia.
Discussion: Successful treatment of COE can be challenging due to the anatomic difficulty and instrumentation limitations. This case highlights a successful treatment of COE with EGD/EUS using fine needle injected contrast-guided stent placement. This technique may have utility in future cases where traditional esophageal stenting technique is not possible.
Disclosures:
Nina Quirk, MS, MD, Nitish Mittal, MD, Yllen Hernandez Blanco, MD, Vaibhav Wadhwa, MD, FACG. P2836 - Effective Antegrade EUS-Guided Puncture With Stent Placement in Completely Obliterated Esophagus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Texas Health, McGovern Medical School, Houston, TX
Introduction: Complete obliterated esophagus (COE) is a consequence of advanced esophageal strictures that is challenging to treat due to technique complexity and high rate of complications. Esophageal stenting has been used in COE; however, there is currently no standard protocol or guideline for COE treatment given the technique’s difficulty and considerable risk of bleeding and perforation. In this report, we describe a unique and successful case of COE recanalization using only anterograde endoscopic ultrasound (EUS)-guided puncture technique with stent placement.
Case Description/Methods: We present a case of 67 year old male with a past medical history of necrotizing gallstone pancreatitis in 4/2017. The patient underwent endoscopic retrograde cholangiopancreatography (ERCP) with stones and sludge removal and biliary stent placement. He subsequently developed complications that lead to numerous abdominal surgeries over the course of a year. On 3/2018 due to inability to tolerate anything by mouth, he underwent esophagogastroduodenoscopy (EGD) with findings of gastro-jejunal (GJ) anastomotic stricture. Several later EGDs demonstrated recurrent esophageal strictures requiring multiple dilations. EGD on 5/2020 showed high grade long esophageal anastomotic stricture status post 7 mm CRE balloon dilation, 80mg Kenalog injection, and partially covered 18mm X 123mm esophageal stent placement under fluoroscopy guidance. He continued to suffer from dysphagia and upper GI bleeds. EGD/EUS on 8/2023 had findings of COE status post EUS-guided access to the distal esophagus with fine needle injection and fluoroscopic confirmation of position. With wire-guided dilation of the tract, placement of an esophageal stent across the proximal extent in the upper esophagus and the distal extent in the distal esophagus within the lumen of the prior stent was achieved. Barium swallow exam confirmed stent placement and no leakage. Recent EGD in 1/2024 showed esophageal stricture status post dilation to 15 mm. After the stenting in 8/2023, the patient has had remarkable clinical and nutritional improvement with resolution of his electrolyte abnormalities and anemia.
Discussion: Successful treatment of COE can be challenging due to the anatomic difficulty and instrumentation limitations. This case highlights a successful treatment of COE with EGD/EUS using fine needle injected contrast-guided stent placement. This technique may have utility in future cases where traditional esophageal stenting technique is not possible.
Figure: Image A shows complete obliteration of esophagus with stricture. Images B-D show progression of stricture opening. Image E shows EUS confirming needle in proper position.
Disclosures:
Nina Quirk indicated no relevant financial relationships.
Nitish Mittal indicated no relevant financial relationships.
Yllen Hernandez Blanco indicated no relevant financial relationships.
Vaibhav Wadhwa indicated no relevant financial relationships.
Nina Quirk, MS, MD, Nitish Mittal, MD, Yllen Hernandez Blanco, MD, Vaibhav Wadhwa, MD, FACG. P2836 - Effective Antegrade EUS-Guided Puncture With Stent Placement in Completely Obliterated Esophagus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
