Monday Poster Session
Category: Interventional Endoscopy
P2839 - Endoscopic Ultrasound-Directed Transgastric ERCP (EDGE) in a Patient With a Prior Gastric Sleeve Converted to Roux-en-Y Gastric Bypass
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SS
Samantha Schweickhardt, MD
Brooke Army Medical Center
San Antonio, TX
Presenting Author(s)
Samantha Schweickhardt, MD1, John Magulick, MD2, Seth Dukes, MD2, John G. Quiles, MD1, Jerome Edelson, MD2
1Brooke Army Medical Center, San Antonio, TX; 2Brooke Army Medical Center, Fort Sam Houston, TX
Introduction: ERCP following roux-en-y gastric bypass (RNYGB) presents a technical challenge, made more feasible with the development of the
EDGE procedure, where an electrocautery-enhanced lumen apposing metal (LAMS) stent is placed to connect the pouch to the
gastric remnant. Prior surgery of the gastric remnant can complicate and even preclude safe LAMS placement. Here, we present a
case of EDGE in a patient with a prior gastric sleeve converted to RNYGB, presenting with papillary stenosis, treated with ERCP with
sphincterotomy and subsequent resolution of her obstruction.
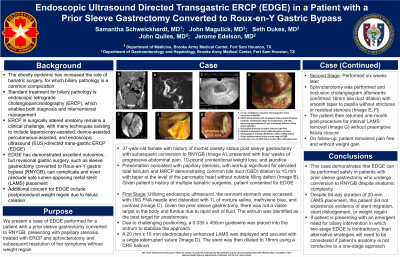
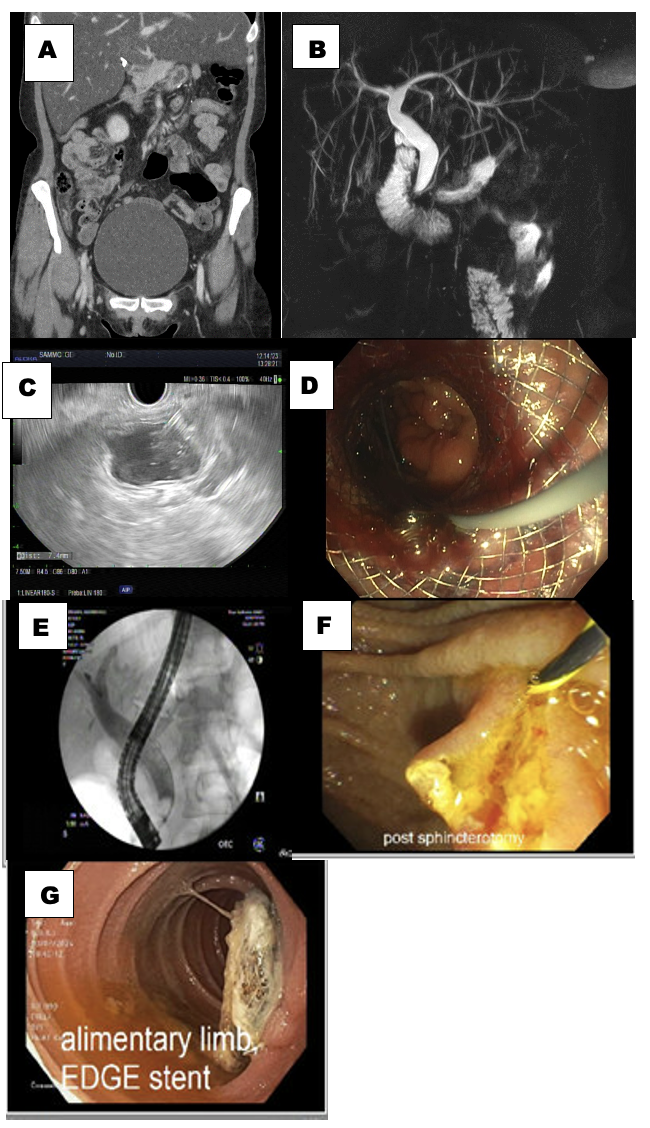
Case Description/Methods: 37-year-old female with history of morbid obesity underwent sleeve gastrectomy with subsequent conversion to RNYGB (Image A)
presented with four weeks of progressive abdominal pain, unintentional weight loss, and jaundice. Labs revealed elevated liver
function tests. MRI/MRCP was notable for CBD dilation to 1.5 cm, suggestive of papillary stenosis (Image B). A 19g FNA needle was
use puncture the lumen and inject contrast to confirm correct placement, followed by a mixture of saline with methylene blue
(Image C). The only safe window was located in the antrum. Due to unstable positioning, a long guide-wire was placed into the
remnant and a 10 mm x 20 mm LAMS was deployed into the antrum over the guide-wire and secured with one suture (Image D). A
two-stage EDGE was planned due to the increased risk of dislodgement given the placement of the stent and as the patient was not.
Approximately 3 weeks later, the patient returned and underwent ERCP with sphincterotomy (Image E, F). The LAMS was removed
three months post-procedure. The patient reported resolution of abdominal pain (Image G). She did not develop significant weight
gain.
Discussion: This case demonstrates that EDGE can be performed safely in patients with prior gastric surgery who undergo conversion to RNYGB.
A staged procedure was chosen due to the non-emergent indication for ERCP and to mitigate stent dislodgement. It is reassuring
that despite complex anatomy and a prolonged time with a LAMS in place, the patient has maintained her post-bariatric surgery
weight and is without evidence of a persistent fistula.
Disclosures:
Samantha Schweickhardt, MD1, John Magulick, MD2, Seth Dukes, MD2, John G. Quiles, MD1, Jerome Edelson, MD2. P2839 - Endoscopic Ultrasound-Directed Transgastric ERCP (EDGE) in a Patient With a Prior Gastric Sleeve Converted to Roux-en-Y Gastric Bypass, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Brooke Army Medical Center, San Antonio, TX; 2Brooke Army Medical Center, Fort Sam Houston, TX
Introduction: ERCP following roux-en-y gastric bypass (RNYGB) presents a technical challenge, made more feasible with the development of the
EDGE procedure, where an electrocautery-enhanced lumen apposing metal (LAMS) stent is placed to connect the pouch to the
gastric remnant. Prior surgery of the gastric remnant can complicate and even preclude safe LAMS placement. Here, we present a
case of EDGE in a patient with a prior gastric sleeve converted to RNYGB, presenting with papillary stenosis, treated with ERCP with
sphincterotomy and subsequent resolution of her obstruction.
Case Description/Methods: 37-year-old female with history of morbid obesity underwent sleeve gastrectomy with subsequent conversion to RNYGB (Image A)
presented with four weeks of progressive abdominal pain, unintentional weight loss, and jaundice. Labs revealed elevated liver
function tests. MRI/MRCP was notable for CBD dilation to 1.5 cm, suggestive of papillary stenosis (Image B). A 19g FNA needle was
use puncture the lumen and inject contrast to confirm correct placement, followed by a mixture of saline with methylene blue
(Image C). The only safe window was located in the antrum. Due to unstable positioning, a long guide-wire was placed into the
remnant and a 10 mm x 20 mm LAMS was deployed into the antrum over the guide-wire and secured with one suture (Image D). A
two-stage EDGE was planned due to the increased risk of dislodgement given the placement of the stent and as the patient was not.
Approximately 3 weeks later, the patient returned and underwent ERCP with sphincterotomy (Image E, F). The LAMS was removed
three months post-procedure. The patient reported resolution of abdominal pain (Image G). She did not develop significant weight
gain.
Discussion: This case demonstrates that EDGE can be performed safely in patients with prior gastric surgery who undergo conversion to RNYGB.
A staged procedure was chosen due to the non-emergent indication for ERCP and to mitigate stent dislodgement. It is reassuring
that despite complex anatomy and a prolonged time with a LAMS in place, the patient has maintained her post-bariatric surgery
weight and is without evidence of a persistent fistula.
Figure: A. CT scan of abdomen and pelvis showing gastric sleeve conversion to RNYGB.
B. MRCP demonstrating mild intrahepatic biliary ductal dilatation, moderate extrahepatic biliary ductal dilatation, and CBD measuring approximately 15 mm in diameter without a filling defect identified.
C. EUS-guided distension of gastric remnant with fluid.
D. Guidewire placement across LAMS into gastric remnant.
E. Cholangiogram showing CBD dilation without filling defects.
F. Biliary sphincterotomy.
G. Endoscopic view of LAMS three months after initial placement.
B. MRCP demonstrating mild intrahepatic biliary ductal dilatation, moderate extrahepatic biliary ductal dilatation, and CBD measuring approximately 15 mm in diameter without a filling defect identified.
C. EUS-guided distension of gastric remnant with fluid.
D. Guidewire placement across LAMS into gastric remnant.
E. Cholangiogram showing CBD dilation without filling defects.
F. Biliary sphincterotomy.
G. Endoscopic view of LAMS three months after initial placement.
Disclosures:
Samantha Schweickhardt indicated no relevant financial relationships.
John Magulick indicated no relevant financial relationships.
Seth Dukes indicated no relevant financial relationships.
John Quiles indicated no relevant financial relationships.
Jerome Edelson indicated no relevant financial relationships.
Samantha Schweickhardt, MD1, John Magulick, MD2, Seth Dukes, MD2, John G. Quiles, MD1, Jerome Edelson, MD2. P2839 - Endoscopic Ultrasound-Directed Transgastric ERCP (EDGE) in a Patient With a Prior Gastric Sleeve Converted to Roux-en-Y Gastric Bypass, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
