Monday Poster Session
Category: Liver
P2881 - Utilization of High Intensity Statins May Protect Against Decompensation in Alcohol-Associated Liver Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- NH
Nariman Hossein-Javaheri, DO
University at Buffalo
Buffalo, NY
Presenting Author(s)
Nariman Hossein-Javaheri, DO1, Himaben Gohil, DO1, Ikjot Singh, MD1, Blake Podger, DO1, Ahmad Abulawi, MD2, Anthony Martinez, MD1
1University at Buffalo, Buffalo, NY; 2Albany Medical Center, Albany, NY
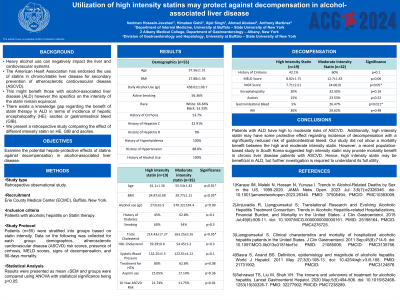
Introduction: Heavy alcohol use can negatively impact the liver and cardiovascular systems. As such, the American Heart Association has endorsed the use of statins in chronic/stable liver disease for secondary prevention of atherosclerotic cardiovascular disease (ASCVD). This might benefit those with alcohol-associated liver disease (ALD) however the specifics on the intensity of the statin remain equivocal. Moreover, there exists a knowledge gap regarding the benefit of statin therapy in ALD in terms of the incidence of hepatic encephalopathy (HE), ascites, or gastrointestinal bleeding (GIB). Herein we present a retrospective study comparing the effect of different intensity statins on HE, GIB, and ascites.
Methods: On admission, 55 patients with hyperlipidemia and ALD on statin therapy were identified. They were stratified into groups based on statin intensity. Data on the following was collected for each group: demographics, atherosclerotic cardiovascular disease (ASCVD) risk scores, presence of cirrhosis, MELD scores, signs of decompensation, and 90-day mortality. Results were presented as mean ±SEM and groups were compared using ANOVA with statistical significance being p< 0.05.
Results: 34.5% (n=19) were on high-intensity statins while 63.6% (n=35) were on moderate-intensity statins. Those on high-intensity statins were significantly older (61.1±1.3 vs 55.5±1.8 years; p< 0.001) with greater ASCVD risk (21.7±2.9 vs 11.7±1.6; p< 0.01). The percentage of cirrhosis (42.1% vs 60%; p=0.1) and MELD scores (8.9±1.7 vs 12.7±1.8; p >0.05) were not significantly different between the two groups; however, those on high-intensity statins had lower rates of HE (20% vs 32.3%; p=0.15), GI bleeding (5% vs 26.4%; p=0.01), and ascites (15% vs 23.5%; p=0.2). There were no mortality benefits in those receiving high vs moderate intensity statins (7.7% vs7.4%; p=0.5).
Discussion: This retrospective study showed patients with ALD have high to moderate risks of ASCVD. Additionally, high-intensity statin may have some protective effect regarding the incidence of decompensation with a significantly reduced risk of GIB. Our study did not show a mortality benefit between the high and moderate-intensity statin. However, a recent population-based study in South Korea suggested that high-intensity statin may provide mortality benefits in chronic liver disease patients with ASCVD. Hence, high-intensity statin may be beneficial in ALD, but further investigation is required to understand its full utility.
Disclosures:
Nariman Hossein-Javaheri, DO1, Himaben Gohil, DO1, Ikjot Singh, MD1, Blake Podger, DO1, Ahmad Abulawi, MD2, Anthony Martinez, MD1. P2881 - Utilization of High Intensity Statins May Protect Against Decompensation in Alcohol-Associated Liver Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University at Buffalo, Buffalo, NY; 2Albany Medical Center, Albany, NY
Introduction: Heavy alcohol use can negatively impact the liver and cardiovascular systems. As such, the American Heart Association has endorsed the use of statins in chronic/stable liver disease for secondary prevention of atherosclerotic cardiovascular disease (ASCVD). This might benefit those with alcohol-associated liver disease (ALD) however the specifics on the intensity of the statin remain equivocal. Moreover, there exists a knowledge gap regarding the benefit of statin therapy in ALD in terms of the incidence of hepatic encephalopathy (HE), ascites, or gastrointestinal bleeding (GIB). Herein we present a retrospective study comparing the effect of different intensity statins on HE, GIB, and ascites.
Methods: On admission, 55 patients with hyperlipidemia and ALD on statin therapy were identified. They were stratified into groups based on statin intensity. Data on the following was collected for each group: demographics, atherosclerotic cardiovascular disease (ASCVD) risk scores, presence of cirrhosis, MELD scores, signs of decompensation, and 90-day mortality. Results were presented as mean ±SEM and groups were compared using ANOVA with statistical significance being p< 0.05.
Results: 34.5% (n=19) were on high-intensity statins while 63.6% (n=35) were on moderate-intensity statins. Those on high-intensity statins were significantly older (61.1±1.3 vs 55.5±1.8 years; p< 0.001) with greater ASCVD risk (21.7±2.9 vs 11.7±1.6; p< 0.01). The percentage of cirrhosis (42.1% vs 60%; p=0.1) and MELD scores (8.9±1.7 vs 12.7±1.8; p >0.05) were not significantly different between the two groups; however, those on high-intensity statins had lower rates of HE (20% vs 32.3%; p=0.15), GI bleeding (5% vs 26.4%; p=0.01), and ascites (15% vs 23.5%; p=0.2). There were no mortality benefits in those receiving high vs moderate intensity statins (7.7% vs7.4%; p=0.5).
Discussion: This retrospective study showed patients with ALD have high to moderate risks of ASCVD. Additionally, high-intensity statin may have some protective effect regarding the incidence of decompensation with a significantly reduced risk of GIB. Our study did not show a mortality benefit between the high and moderate-intensity statin. However, a recent population-based study in South Korea suggested that high-intensity statin may provide mortality benefits in chronic liver disease patients with ASCVD. Hence, high-intensity statin may be beneficial in ALD, but further investigation is required to understand its full utility.
Disclosures:
Nariman Hossein-Javaheri indicated no relevant financial relationships.
Himaben Gohil indicated no relevant financial relationships.
Ikjot Singh indicated no relevant financial relationships.
Blake Podger indicated no relevant financial relationships.
Ahmad Abulawi indicated no relevant financial relationships.
Anthony Martinez: Abbvie – Consultant, Speakers Bureau. Arbutus – Consultant. Braeburn – Speakers Bureau. Gilead – Consultant, Speakers Bureau. Madrigal – Speakers Bureau. Roche – Consultant. Sirtex – Consultant. VBI – Consultant.
Nariman Hossein-Javaheri, DO1, Himaben Gohil, DO1, Ikjot Singh, MD1, Blake Podger, DO1, Ahmad Abulawi, MD2, Anthony Martinez, MD1. P2881 - Utilization of High Intensity Statins May Protect Against Decompensation in Alcohol-Associated Liver Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
