Tuesday Poster Session
Category: GI Bleeding
P4243 - Gastrosplenic Collaterals Disguised as Gastric Varices: An Rare Case of Upper Gastrointestinal Bleed
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ryan Burden, MD, MBA
Tulane School of Medicine
New Orleans, LA
Presenting Author(s)
Ryan Burden, MD, MBA, Samantha Wu, MD, Michael Conner, MD
Tulane School of Medicine, New Orleans, LA
Introduction: Management of upper gastrointestinal bleeding (UGIB) relies on accurate diagnosis to guide treatment. We present a case of recurrent melena and symptomatic anemia, initially suspected as gastric varices. Further investigation revealed gastrosplenic artery collaterals as the bleeding source, leading to successful treatment with transarterial embolization.
Case Description/Methods: A 60-year-old man presented with a 3-week-history of recurrent melena. He had no medical history apart from a motor vehicle accident one month prior that was complicated by a splenic hematoma status post splenic artery embolization (SAE). He described black stool but denied abdominal pain, known liver disease, personal or family history of malignancy, or alcohol use. He had been hospitalized three times prior for melena with two EGDs that were unremarkable. He was afebrile, hemodynamically stable and his physical examination was unrevealing. Hemoglobin was 8.4 g/dL. Initial CT angiogram (CTA) showed a subacute splenic hematoma with no evidence of active hemorrhage. No active bleeding, old blood, or stigmata of recent bleeding were found on repeat EGD. Colonoscopy demonstrated diverticulosis in the sigmoid colon and blood in the entire examined colon. He continued to have recurrent melena and down trending hemoglobin. Repeat CTA on day four of admission showed no evidence of contrast extravasation but did show hyperdense material within the stomach concerning for clotted blood. The decision was made to repeat an EGD which revealed hematin throughout the stomach and bulging mucosa in the gastric fundus which was interpreted as gastric varices with stigmata of recent bleeding. However, on further review of the CTA, there was high suspicion that the presumed gastric varices were instead aberrant arterial vessels related to his prior SAE. Angiogram confirmed the presence of a dense tangle of collateral arteries along the fundus of the stomach and which appeared to be eroding through the mucosa; these were urgently embolized. The patient's hemoglobin stabilized after embolization with no further recurrence of GI bleeding observed.
Discussion: Gastrosplenic collaterals can form acutely after prior successful SAE and may predispose to erosion of gastric lumen and subsequent upper GIB. Suspicion for atypical sources of upper GIB should remain high in patients with negative endoscopic studies and prior history of SAE, including occult formation of splenic collaterals. Embolization appears to be a successful therapeutic approach.
Disclosures:
Ryan Burden, MD, MBA, Samantha Wu, MD, Michael Conner, MD. P4243 - Gastrosplenic Collaterals Disguised as Gastric Varices: An Rare Case of Upper Gastrointestinal Bleed, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Tulane School of Medicine, New Orleans, LA
Introduction: Management of upper gastrointestinal bleeding (UGIB) relies on accurate diagnosis to guide treatment. We present a case of recurrent melena and symptomatic anemia, initially suspected as gastric varices. Further investigation revealed gastrosplenic artery collaterals as the bleeding source, leading to successful treatment with transarterial embolization.
Case Description/Methods: A 60-year-old man presented with a 3-week-history of recurrent melena. He had no medical history apart from a motor vehicle accident one month prior that was complicated by a splenic hematoma status post splenic artery embolization (SAE). He described black stool but denied abdominal pain, known liver disease, personal or family history of malignancy, or alcohol use. He had been hospitalized three times prior for melena with two EGDs that were unremarkable. He was afebrile, hemodynamically stable and his physical examination was unrevealing. Hemoglobin was 8.4 g/dL. Initial CT angiogram (CTA) showed a subacute splenic hematoma with no evidence of active hemorrhage. No active bleeding, old blood, or stigmata of recent bleeding were found on repeat EGD. Colonoscopy demonstrated diverticulosis in the sigmoid colon and blood in the entire examined colon. He continued to have recurrent melena and down trending hemoglobin. Repeat CTA on day four of admission showed no evidence of contrast extravasation but did show hyperdense material within the stomach concerning for clotted blood. The decision was made to repeat an EGD which revealed hematin throughout the stomach and bulging mucosa in the gastric fundus which was interpreted as gastric varices with stigmata of recent bleeding. However, on further review of the CTA, there was high suspicion that the presumed gastric varices were instead aberrant arterial vessels related to his prior SAE. Angiogram confirmed the presence of a dense tangle of collateral arteries along the fundus of the stomach and which appeared to be eroding through the mucosa; these were urgently embolized. The patient's hemoglobin stabilized after embolization with no further recurrence of GI bleeding observed.
Discussion: Gastrosplenic collaterals can form acutely after prior successful SAE and may predispose to erosion of gastric lumen and subsequent upper GIB. Suspicion for atypical sources of upper GIB should remain high in patients with negative endoscopic studies and prior history of SAE, including occult formation of splenic collaterals. Embolization appears to be a successful therapeutic approach.
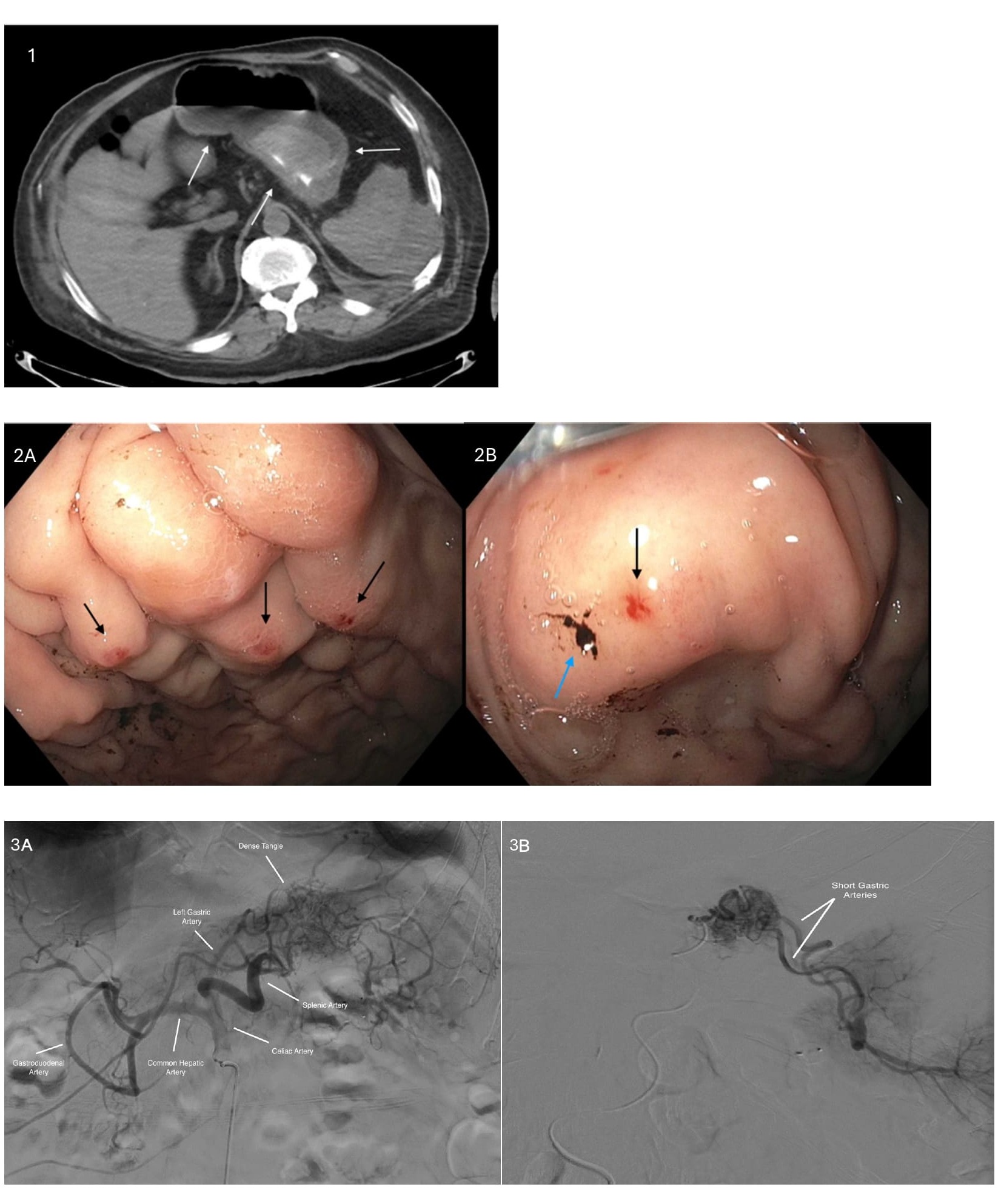
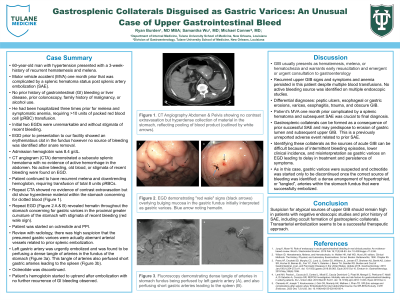
Figure: Figure 1. CT Angiography Abdomen & Pelvis showing no contrast extravasation but hyperdense collection of material in the stomach, reflecting pooling of blood product (outlined by white arrows).
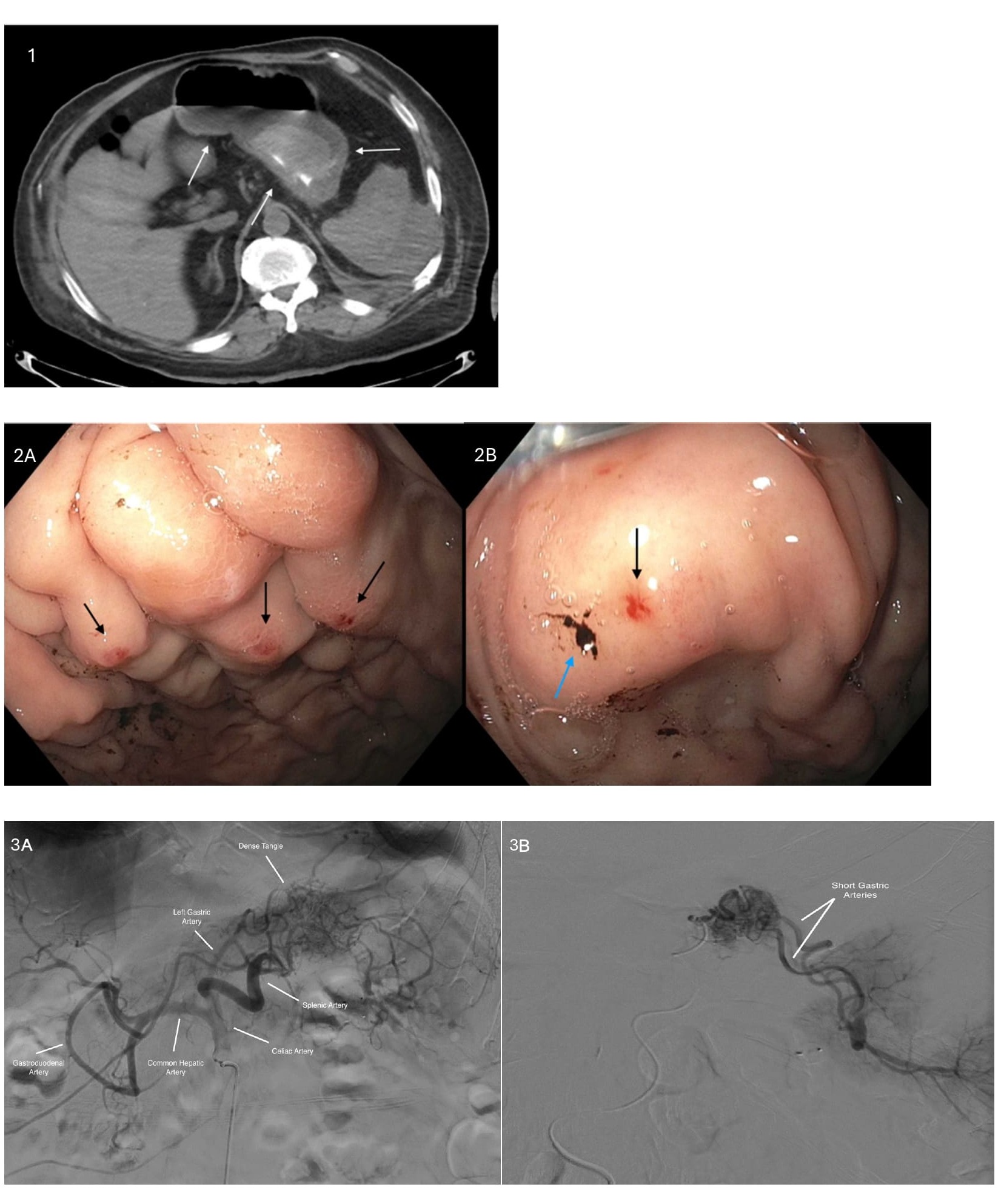
Figure 2A and 2B. EGD demonstrating "red wale" signs (black arrows) overlying bulging mucosa in the gastric fundus initially interpreted as gastric varices. Blue arrow noting hematin.
Figure 3A and 3B. Fluoroscopy demonstrating dense tangle of arteries in the gastric fundus being perfused by the left gastric artery (A), and perfusing short gastric arteries leading to the spleen (B).
Figure 2A and 2B. EGD demonstrating "red wale" signs (black arrows) overlying bulging mucosa in the gastric fundus initially interpreted as gastric varices. Blue arrow noting hematin.
Figure 3A and 3B. Fluoroscopy demonstrating dense tangle of arteries in the gastric fundus being perfused by the left gastric artery (A), and perfusing short gastric arteries leading to the spleen (B).
Disclosures:
Ryan Burden indicated no relevant financial relationships.
Samantha Wu indicated no relevant financial relationships.
Michael Conner indicated no relevant financial relationships.
Ryan Burden, MD, MBA, Samantha Wu, MD, Michael Conner, MD. P4243 - Gastrosplenic Collaterals Disguised as Gastric Varices: An Rare Case of Upper Gastrointestinal Bleed, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
