Tuesday Poster Session
Category: IBD
P4272 - A Quality Improvement Initiative to Bridge Gaps in Patient Access to IBD Therapies
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Erica R. Cohen, MD
Director of IBD Chronic Care Program and Research
Capital Digestive Care
Chevy Chase, MD
Presenting Author(s)
Erica R. Cohen, MD1, Frank I. Scott, MD2, Jeffrey Carter, PhD3, Laura Simone, PhD3, Marykate Nelson, PhD3
1Capital Digestive Care, Chevy Chase, MD; 2University of Colorado Anschutz Medical Campus, Aurora, CO; 3PRIME Education, New York, NY
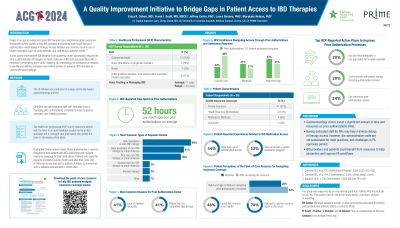
Introduction: Delays in access to evidenced-based IBD therapies can compromise patient outcomes. Applying quality improvement (QI) methodology, we conducted an initiative to identify and address managed care-related barriers to advanced IBD therapies.
Methods: The QI cohort comprised gastroenterology clinicians at a large community-based gastroenterology group practice, along with administrative staff with dedicated roles in managing prior authorizations (PAs). Team members completed a survey to assess managed care-related processes and participated in an audit-feedback session led by an IBD specialist and a managed care pharmacist who guided participants in reviewing the survey data and developing action plans. As part of the QI intervention phase, clinics implemented a resource designed to help patients with IBD understand and navigate insurance coverage for their medications.
Results: A total of 29 team members completed the baseline survey. On average, team members estimated that their team spends 52 hours per month on PAs. Team members encountered PA-related delays/denials most often when requesting increased dosing for anti-TNF biologics (48%) or non-TNF biologics/small molecule therapies (41%) and when requesting non-TNF biologics/small molecule therapies for first-line treatment (38%). Only 45% and 31% of team members had high/very high confidence in navigating PA requirements and patient assistance programs, respectively. The top 2 strategies team members planned to implement after the audit-feedback session to improve their teams’ PA processes were use of pre-filled templates (29%) and communication with payers during the PA process (29%).
Among patients who utilized the managed care resource (n=53), 34% had experienced a PA denial for their IBD medication and 53% had accessed patient assistance programs. Only 28% of patients felt confident/very confident in navigating insurance approval processes, which increased to 34% after accessing the resource. Many patients found the resource helpful/very helpful (48%) and planned to use the resource in the future (78%).
Discussion: Gastroenterology clinics invest a significant amount of time and resources on PAs. Having dedicated staff for PAs may help minimize delays in therapy access, but the administrative costs are not sustainable for most practices and challenges in PA approvals persist. IBD providers and patients could benefit from resources to help streamline and improve PA workflows.
Disclosures:
Erica R. Cohen, MD1, Frank I. Scott, MD2, Jeffrey Carter, PhD3, Laura Simone, PhD3, Marykate Nelson, PhD3. P4272 - A Quality Improvement Initiative to Bridge Gaps in Patient Access to IBD Therapies, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Capital Digestive Care, Chevy Chase, MD; 2University of Colorado Anschutz Medical Campus, Aurora, CO; 3PRIME Education, New York, NY
Introduction: Delays in access to evidenced-based IBD therapies can compromise patient outcomes. Applying quality improvement (QI) methodology, we conducted an initiative to identify and address managed care-related barriers to advanced IBD therapies.
Methods: The QI cohort comprised gastroenterology clinicians at a large community-based gastroenterology group practice, along with administrative staff with dedicated roles in managing prior authorizations (PAs). Team members completed a survey to assess managed care-related processes and participated in an audit-feedback session led by an IBD specialist and a managed care pharmacist who guided participants in reviewing the survey data and developing action plans. As part of the QI intervention phase, clinics implemented a resource designed to help patients with IBD understand and navigate insurance coverage for their medications.
Results: A total of 29 team members completed the baseline survey. On average, team members estimated that their team spends 52 hours per month on PAs. Team members encountered PA-related delays/denials most often when requesting increased dosing for anti-TNF biologics (48%) or non-TNF biologics/small molecule therapies (41%) and when requesting non-TNF biologics/small molecule therapies for first-line treatment (38%). Only 45% and 31% of team members had high/very high confidence in navigating PA requirements and patient assistance programs, respectively. The top 2 strategies team members planned to implement after the audit-feedback session to improve their teams’ PA processes were use of pre-filled templates (29%) and communication with payers during the PA process (29%).
Among patients who utilized the managed care resource (n=53), 34% had experienced a PA denial for their IBD medication and 53% had accessed patient assistance programs. Only 28% of patients felt confident/very confident in navigating insurance approval processes, which increased to 34% after accessing the resource. Many patients found the resource helpful/very helpful (48%) and planned to use the resource in the future (78%).
Discussion: Gastroenterology clinics invest a significant amount of time and resources on PAs. Having dedicated staff for PAs may help minimize delays in therapy access, but the administrative costs are not sustainable for most practices and challenges in PA approvals persist. IBD providers and patients could benefit from resources to help streamline and improve PA workflows.
Disclosures:
Erica Cohen: Abbvie – Consultant, Speakers Bureau. Eli Lilly & Co – Speakers Bureau. Johnson & Johnson – Consultant, Speakers Bureau. Pfizer – Consultant. Takeda – Speakers Bureau.
Frank Scott: Crohn's and Colitis Foundation – Grant/Research Support. Takeda Pharmaceuticals – Grant/Research Support.
Jeffrey Carter indicated no relevant financial relationships.
Laura Simone indicated no relevant financial relationships.
Marykate Nelson indicated no relevant financial relationships.
Erica R. Cohen, MD1, Frank I. Scott, MD2, Jeffrey Carter, PhD3, Laura Simone, PhD3, Marykate Nelson, PhD3. P4272 - A Quality Improvement Initiative to Bridge Gaps in Patient Access to IBD Therapies, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
