Tuesday Poster Session
Category: IBD
P4286 - Statins and the Risk of Colorectal Cancer in Patients With Inflammatory Bowel Diseases: A Systemic Review and Meta-Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Joelle Sleiman, MD
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Joelle Sleiman, MD1, Un Jung Lee, PhD2, Brendan Plann-Curley, 3, Peter Khouri, MD4, Cristina Sison, PhD2, Liliane Deeb, MD1
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Biostatistics Unit, Office of Academic Affairs, Northwell Health, Staten Island, NY; 3Northwell, New Hyde Park, NY and Medical Library, Staten Island University Hospital, Staten Island, NY; 4SUNY Downstate Health Sciences University, Staten Island, NY
Introduction: Statins have been reported to decrease the risk of colorectal cancer (CRC) development in the general population. However, this benefit in patients with Inflammatory Bowel Disease (IBD), a high-risk population for CRC, remains inconclusive to date. We aim to investigate the association between statin therapy and the risk of developing CRC in patients with IBD.
Methods: We conducted a systematic literature search on PubMed, EMBASE and Web of Science using the primary keywords: Inflammatory Bowel Disease, Ulcerative Colitis, Crohn's Disease, Inflammatory Colitis AND Colon, Colorectal, Rectal, Carcinoma, Cancer, Neoplasia, AND Hydroxymethylglutaryl-CoA Reductase Inhibitor, HMG CoA, Statin. After deduplication, 324 studies were screened. Studies were included if they evaluated the association between statin use and CRC in patients with IBD and reported Odds Ratio(OR) or Hazard Ratio(HR). The primary endpoints were developing CRC(OR) and time-to-CRC(HR). A meta-analysis(MA) was performed using fixed/random-effects model to estimate the overall effect using OR and HR separately. Test for heterogeneity between studies was performed. A funnel plot was generated to assess publication bias. All analyses were conducted (alpha=0.05) using R(V4.3.0).
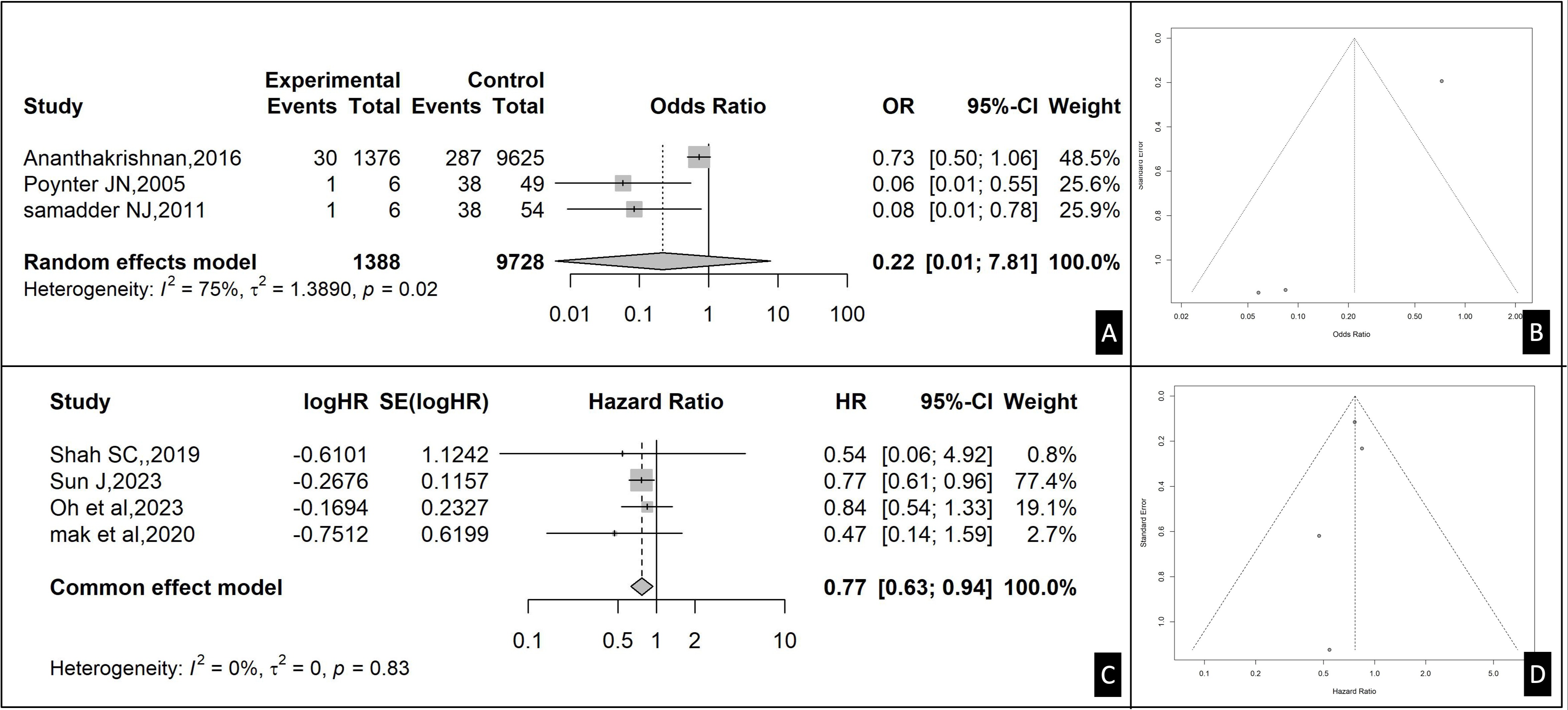
Results: Seven studies involving 59,596 patients were eligible for this MA; 3 for OR(11,116 pts), and 4 for HR(48,480 pts).
1- OR:The pooled effect size, based on the random effects model, is OR=0.22 (95%CI:0.01–7.81). This indicates that the odds of developing CRC in statin-users is 78% lower than non-users, however this was not significant(p=0.21)(Fig1A). The funnel plot is asymmetric indicating possible publication bias(Fig1B).
2- HR:The pooled effect size, based on the fixed effects model, is HR=0.77 (95%CI:0.63–0.94). The result is significant(p< 0.05) indicating that the hazard of developing CRC in statin-users is 23% lower than non-users(Fig1C). The funnel plot is symmetric indicating low publication bias(Fig1D).
The HR analysis was based on more patients, included studies that reported adjusted HR, and considered the time-to-development of CRC and other confounding factors, thus enhancing its reliability.
Discussion: Based on the HR analysis, our findings suggest that statin use was associated with a significant decrease in the hazard of developing CRC in IBD patients. Large RCTs are warranted to clarify the duration of statin use and their chemopreventive effects independent of variables like targeted therapy for the chronic mucosal inflammation.
Disclosures:
Joelle Sleiman, MD1, Un Jung Lee, PhD2, Brendan Plann-Curley, 3, Peter Khouri, MD4, Cristina Sison, PhD2, Liliane Deeb, MD1. P4286 - Statins and the Risk of Colorectal Cancer in Patients With Inflammatory Bowel Diseases: A Systemic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Biostatistics Unit, Office of Academic Affairs, Northwell Health, Staten Island, NY; 3Northwell, New Hyde Park, NY and Medical Library, Staten Island University Hospital, Staten Island, NY; 4SUNY Downstate Health Sciences University, Staten Island, NY
Introduction: Statins have been reported to decrease the risk of colorectal cancer (CRC) development in the general population. However, this benefit in patients with Inflammatory Bowel Disease (IBD), a high-risk population for CRC, remains inconclusive to date. We aim to investigate the association between statin therapy and the risk of developing CRC in patients with IBD.
Methods: We conducted a systematic literature search on PubMed, EMBASE and Web of Science using the primary keywords: Inflammatory Bowel Disease, Ulcerative Colitis, Crohn's Disease, Inflammatory Colitis AND Colon, Colorectal, Rectal, Carcinoma, Cancer, Neoplasia, AND Hydroxymethylglutaryl-CoA Reductase Inhibitor, HMG CoA, Statin. After deduplication, 324 studies were screened. Studies were included if they evaluated the association between statin use and CRC in patients with IBD and reported Odds Ratio(OR) or Hazard Ratio(HR). The primary endpoints were developing CRC(OR) and time-to-CRC(HR). A meta-analysis(MA) was performed using fixed/random-effects model to estimate the overall effect using OR and HR separately. Test for heterogeneity between studies was performed. A funnel plot was generated to assess publication bias. All analyses were conducted (alpha=0.05) using R(V4.3.0).
Results: Seven studies involving 59,596 patients were eligible for this MA; 3 for OR(11,116 pts), and 4 for HR(48,480 pts).
1- OR:The pooled effect size, based on the random effects model, is OR=0.22 (95%CI:0.01–7.81). This indicates that the odds of developing CRC in statin-users is 78% lower than non-users, however this was not significant(p=0.21)(Fig1A). The funnel plot is asymmetric indicating possible publication bias(Fig1B).
2- HR:The pooled effect size, based on the fixed effects model, is HR=0.77 (95%CI:0.63–0.94). The result is significant(p< 0.05) indicating that the hazard of developing CRC in statin-users is 23% lower than non-users(Fig1C). The funnel plot is symmetric indicating low publication bias(Fig1D).
The HR analysis was based on more patients, included studies that reported adjusted HR, and considered the time-to-development of CRC and other confounding factors, thus enhancing its reliability.
Discussion: Based on the HR analysis, our findings suggest that statin use was associated with a significant decrease in the hazard of developing CRC in IBD patients. Large RCTs are warranted to clarify the duration of statin use and their chemopreventive effects independent of variables like targeted therapy for the chronic mucosal inflammation.
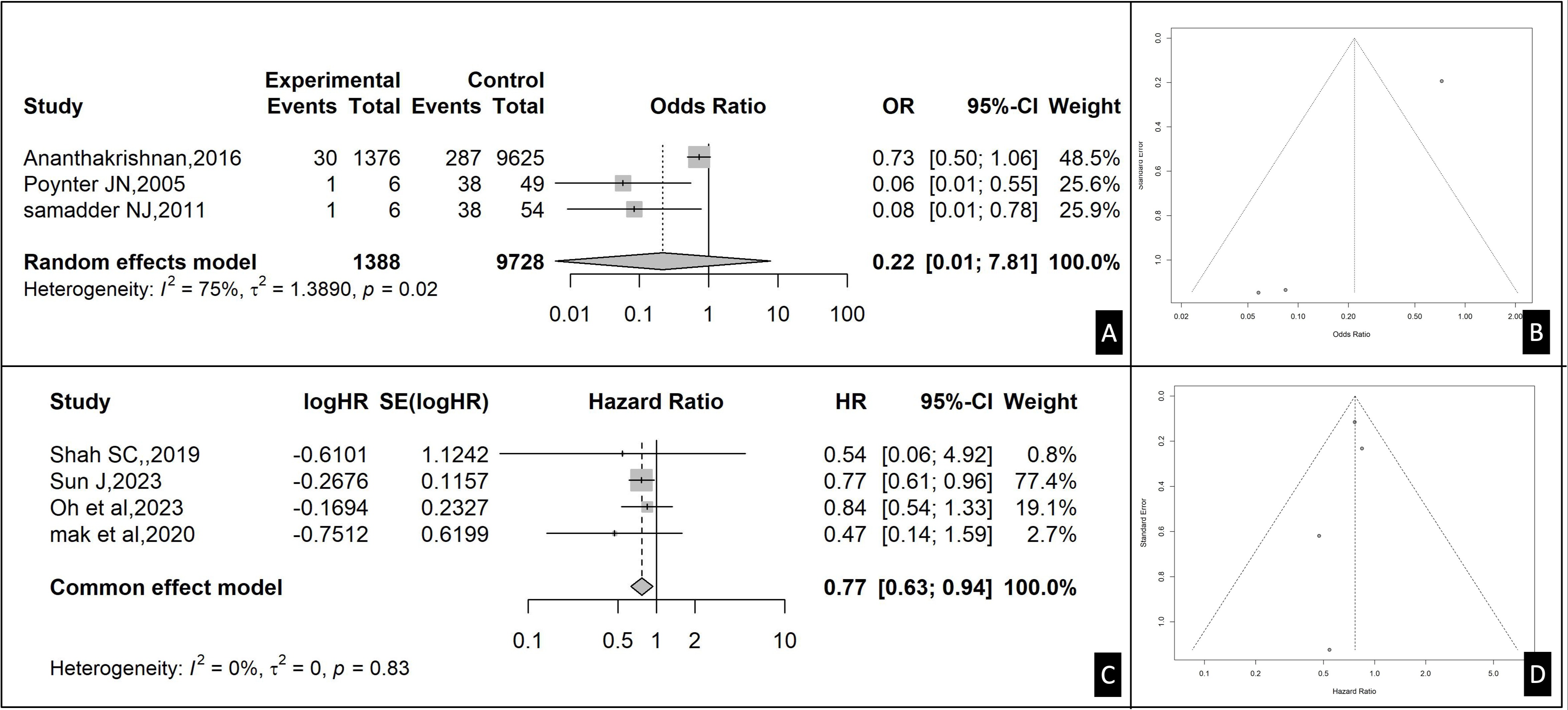
Figure: Figure 1: Overall effect of OR and HR separately and publication bias. A- Forest plot of overall effect for OR. B- Funnel Plot-Publication Bias (Odds Ratio). C- Forest plot of overall effect for HR. D- Funnel Plot-Publication Bias (Hazard Ratio)
Disclosures:
Joelle Sleiman indicated no relevant financial relationships.
Un Jung Lee indicated no relevant financial relationships.
Brendan Plann-Curley indicated no relevant financial relationships.
Peter Khouri indicated no relevant financial relationships.
Cristina Sison indicated no relevant financial relationships.
Liliane Deeb indicated no relevant financial relationships.
Joelle Sleiman, MD1, Un Jung Lee, PhD2, Brendan Plann-Curley, 3, Peter Khouri, MD4, Cristina Sison, PhD2, Liliane Deeb, MD1. P4286 - Statins and the Risk of Colorectal Cancer in Patients With Inflammatory Bowel Diseases: A Systemic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
