Tuesday Poster Session
Category: IBD
P4290 - Withholding a Diet for Hospitalized Patients With IBD Flares is Common but Does Not Improve IBD-Related Outcomes
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- VP
Vincent Phan, MD
University of Texas at Austin Dell Medical School
Austin, TX
Presenting Author(s)
Vincent Phan, MD1, Jonathan Espinoza, MD1, Ariel Hurwitz, MD1, Natalie Malluru, BA1, Chandershekhar Shori, MPH2, Clara DiVincenzo, RD1, Linda A. Feagins, MD, FACG1
1University of Texas at Austin Dell Medical School, Austin, TX; 2University of Central Florida College of Medicine, Orlando, FL
Introduction: There are limited indications for bowel rest for hospitalized patients with an IBD flare, particularly in patients with inflammatory disease (i.e. no obstruction, abscess or fistula). A major concern in treating hospitalized patients with IBD is the prevention and treatment of malnutrition, as untreated malnutrition may worsen the prognosis, complication rates, mortality, and quality of life of patients with IBD. However, it is still common practice for patients to have diets withheld during hospitalization. We aimed to assess how often withholding a diet occurs and its impact on important IBD-related outcomes.
Methods: Patients with IBD flares between 2015 and 2020 who were admitted to one of 6 hospitals within a large urban hospital network were included. Patients with obstruction, active intra-abdominal fistulas or abscess, elective surgery, or new diagnoses of IBD were excluded. Time spent nil per os (NPO) or on a clear liquid diet (CLD) was calculated as a percentage of the total length of stay and analyzed by quartiles of lowest to highest percentage of the hospitalization spent NPO/CLD. Fisher’s test was used for categorical variables. A p-value of < 0.05 was considered statistically significant.
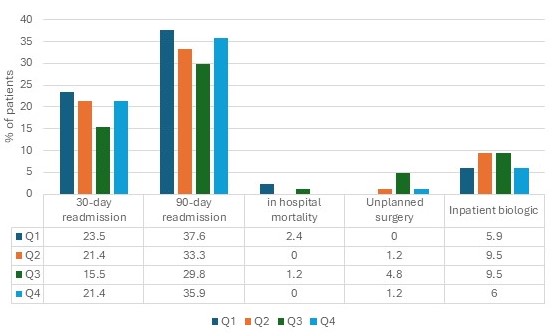
Results: 337 patients (148 CD, 185 UC, 4 IBDU) were included. The cohort had an average age of 38.2 years and was 44.9% male (see table). Most of the cohort (91.4%) spent some portion of the hospitalization with NPO/CLD orders averaging 35.4% of the hospitalization without a diet. The 30-day readmission rates, 90-day readmission rates, in hospital mortality, need for unplanned surgery, or inpatient treatment with a biologic was not different between those in the lowest and highest quartiles. No trends were seen across the quartiles (see figure). Similar findings were seen on subgroup analysis of patients with CD and UC.
Discussion: We found that withholding a diet occurs in most hospital admissions for patients with IBD flares and encompasses, on average, a third of their stay. Not surprisingly, increased NPO/CLD time did not improve readmission rates, mortality, need for surgery, or need for inpatient treatment with a biologic. Based on this data, we speculate that empiric treatment with bowel rest is not beneficial for hospitalized IBD patients with inflammatory symptoms.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Vincent Phan, MD1, Jonathan Espinoza, MD1, Ariel Hurwitz, MD1, Natalie Malluru, BA1, Chandershekhar Shori, MPH2, Clara DiVincenzo, RD1, Linda A. Feagins, MD, FACG1. P4290 - Withholding a Diet for Hospitalized Patients With IBD Flares is Common but Does Not Improve IBD-Related Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas at Austin Dell Medical School, Austin, TX; 2University of Central Florida College of Medicine, Orlando, FL
Introduction: There are limited indications for bowel rest for hospitalized patients with an IBD flare, particularly in patients with inflammatory disease (i.e. no obstruction, abscess or fistula). A major concern in treating hospitalized patients with IBD is the prevention and treatment of malnutrition, as untreated malnutrition may worsen the prognosis, complication rates, mortality, and quality of life of patients with IBD. However, it is still common practice for patients to have diets withheld during hospitalization. We aimed to assess how often withholding a diet occurs and its impact on important IBD-related outcomes.
Methods: Patients with IBD flares between 2015 and 2020 who were admitted to one of 6 hospitals within a large urban hospital network were included. Patients with obstruction, active intra-abdominal fistulas or abscess, elective surgery, or new diagnoses of IBD were excluded. Time spent nil per os (NPO) or on a clear liquid diet (CLD) was calculated as a percentage of the total length of stay and analyzed by quartiles of lowest to highest percentage of the hospitalization spent NPO/CLD. Fisher’s test was used for categorical variables. A p-value of < 0.05 was considered statistically significant.
Results: 337 patients (148 CD, 185 UC, 4 IBDU) were included. The cohort had an average age of 38.2 years and was 44.9% male (see table). Most of the cohort (91.4%) spent some portion of the hospitalization with NPO/CLD orders averaging 35.4% of the hospitalization without a diet. The 30-day readmission rates, 90-day readmission rates, in hospital mortality, need for unplanned surgery, or inpatient treatment with a biologic was not different between those in the lowest and highest quartiles. No trends were seen across the quartiles (see figure). Similar findings were seen on subgroup analysis of patients with CD and UC.
Discussion: We found that withholding a diet occurs in most hospital admissions for patients with IBD flares and encompasses, on average, a third of their stay. Not surprisingly, increased NPO/CLD time did not improve readmission rates, mortality, need for surgery, or need for inpatient treatment with a biologic. Based on this data, we speculate that empiric treatment with bowel rest is not beneficial for hospitalized IBD patients with inflammatory symptoms.
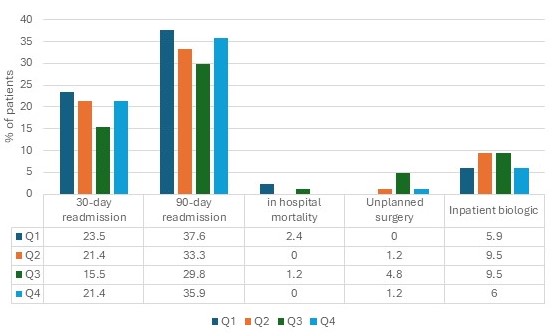
Figure: Outcomes analyzed by quartiles based on time spent NPO or on a CLD as a percentage of the total length of hospital stay. Quartile 1 was the lowest percentage spent with NPO or CLD while quartile 4 was the highest percentage of time spent NPO or CLD.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Vincent Phan indicated no relevant financial relationships.
Jonathan Espinoza indicated no relevant financial relationships.
Ariel Hurwitz indicated no relevant financial relationships.
Natalie Malluru indicated no relevant financial relationships.
Chandershekhar Shori indicated no relevant financial relationships.
Clara DiVincenzo indicated no relevant financial relationships.
Linda Feagins: CorEvitas – Study Site for Research Study. Takeda – Local Study Site for research study.
Vincent Phan, MD1, Jonathan Espinoza, MD1, Ariel Hurwitz, MD1, Natalie Malluru, BA1, Chandershekhar Shori, MPH2, Clara DiVincenzo, RD1, Linda A. Feagins, MD, FACG1. P4290 - Withholding a Diet for Hospitalized Patients With IBD Flares is Common but Does Not Improve IBD-Related Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
