Tuesday Poster Session
Category: IBD
P4298 - Long-Term Cardiovascular Outcomes Among Patients With Microscopic Colitis: A Propensity Score Matched Analysis from Global Federated Health Research Network
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jordan Carty, MD
Albert Einstein Medical Center
Philadelphia, PA
Presenting Author(s)
Jordan Carty, MD1, Phuuwadith Wattanachayakul, MD1, Evan Isaacs, DO2, Oluwanifemi Balogun, MD1, Jessica Genkil, DO3, Tinsae Anebo, MD1, Karecia Byfield, MBBS1, Sahana Tito, MD4, Colton F. Jones, MBBS1, Carlo Gabriel C. Casipit, MD1, Michael Goldberg, DO1
1Albert Einstein Medical Center, Philadelphia, PA; 2Einstein Healthcare Network, Philadelphia, PA; 3Jefferson Einstein, Huntingdon Valley, PA; 4Albert Einstein Medical Center, Philadephia, PA
Introduction: Microscopic colitis is associated with several systemic conditions such as acute pancreatitis, type 1 diabetes mellitus, and thyroid disease. However, there exists a paucity of data on the relationship between cardiovascular outcomes and microscopic colitis.
Methods: A retrospective cohort study was conducted using the US Collaborative Network TriNetX, covering January 2000 to December 2023. Patients with microscopic colitis were identified and compared to healthy individuals without the condition. The microscopic colitis group was propensity-matched with the control group based on age, sex, race, and comorbidities. We followed these patients for five years to assess outcomes, including incidents of heart failure (HF), ischemic stroke, acute myocardial infarction (AMI), pulmonary embolism (PE), atrial fibrillation (AF), and hospitalizations.
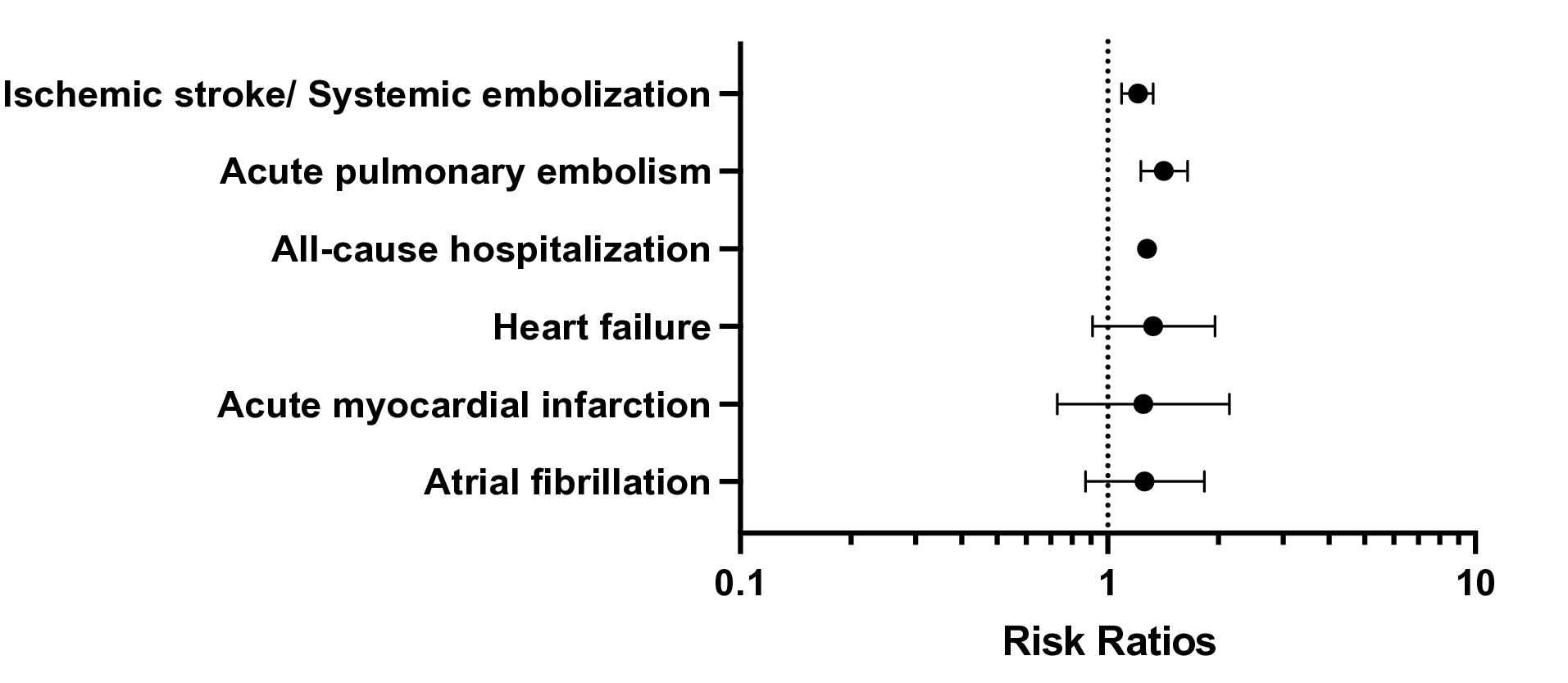
Results: Each cohort consisted of 39,117 patients after propensity score matching, with similar baseline characteristics. The average age was 59.6 years in both groups, and 75% of each cohort was female. In the microscopic colitis cohort, the ethnicity distribution was 88% White, 2.5% Hispanic, and 1.9% African American. In contrast, the control group had an ethnicity distribution of 61.5% White, 10.3% African American, and 5.2% Hispanic. Our analysis found that within five years, patients with microscopic colitis had a significantly higher risk of ischemic stroke/systemic embolization (RR: 1.21, 95% CI: 1.09-1.33, P = 0.002), acute pulmonary embolism (RR: 1.42, 95% CI: 1.23-1.65, P < 0.001), and all-cause hospitalization (RR: 1.28, 95% CI: 1.24-1.31, P < 0.001). Although the observed risks for incident of HF (RR: 1.33, 95% CI: 0.91-1.96, P = 0.143), AMI (RR: 1.25, 95% CI: 0.73-2.14, P = 0.414), and AF (RR: 1.26, 95% CI: 0.87-1.83, P = 0.221) were higher, they did not reach statistical significance.
Discussion: Our study revealed that individuals diagnosed with microscopic colitis face heightened long-term susceptibility to acute pulmonary embolism, ischemic stroke/systemic embolization, and all-cause hospitalization. Additional longitudinal cohort studies are imperative to delve into the intricate interplay between microscopic colitis and cardiovascular outcomes, as well as to devise prospective risk prediction methodologies.
Disclosures:
Jordan Carty, MD1, Phuuwadith Wattanachayakul, MD1, Evan Isaacs, DO2, Oluwanifemi Balogun, MD1, Jessica Genkil, DO3, Tinsae Anebo, MD1, Karecia Byfield, MBBS1, Sahana Tito, MD4, Colton F. Jones, MBBS1, Carlo Gabriel C. Casipit, MD1, Michael Goldberg, DO1. P4298 - Long-Term Cardiovascular Outcomes Among Patients With Microscopic Colitis: A Propensity Score Matched Analysis from Global Federated Health Research Network, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Albert Einstein Medical Center, Philadelphia, PA; 2Einstein Healthcare Network, Philadelphia, PA; 3Jefferson Einstein, Huntingdon Valley, PA; 4Albert Einstein Medical Center, Philadephia, PA
Introduction: Microscopic colitis is associated with several systemic conditions such as acute pancreatitis, type 1 diabetes mellitus, and thyroid disease. However, there exists a paucity of data on the relationship between cardiovascular outcomes and microscopic colitis.
Methods: A retrospective cohort study was conducted using the US Collaborative Network TriNetX, covering January 2000 to December 2023. Patients with microscopic colitis were identified and compared to healthy individuals without the condition. The microscopic colitis group was propensity-matched with the control group based on age, sex, race, and comorbidities. We followed these patients for five years to assess outcomes, including incidents of heart failure (HF), ischemic stroke, acute myocardial infarction (AMI), pulmonary embolism (PE), atrial fibrillation (AF), and hospitalizations.
Results: Each cohort consisted of 39,117 patients after propensity score matching, with similar baseline characteristics. The average age was 59.6 years in both groups, and 75% of each cohort was female. In the microscopic colitis cohort, the ethnicity distribution was 88% White, 2.5% Hispanic, and 1.9% African American. In contrast, the control group had an ethnicity distribution of 61.5% White, 10.3% African American, and 5.2% Hispanic. Our analysis found that within five years, patients with microscopic colitis had a significantly higher risk of ischemic stroke/systemic embolization (RR: 1.21, 95% CI: 1.09-1.33, P = 0.002), acute pulmonary embolism (RR: 1.42, 95% CI: 1.23-1.65, P < 0.001), and all-cause hospitalization (RR: 1.28, 95% CI: 1.24-1.31, P < 0.001). Although the observed risks for incident of HF (RR: 1.33, 95% CI: 0.91-1.96, P = 0.143), AMI (RR: 1.25, 95% CI: 0.73-2.14, P = 0.414), and AF (RR: 1.26, 95% CI: 0.87-1.83, P = 0.221) were higher, they did not reach statistical significance.
Discussion: Our study revealed that individuals diagnosed with microscopic colitis face heightened long-term susceptibility to acute pulmonary embolism, ischemic stroke/systemic embolization, and all-cause hospitalization. Additional longitudinal cohort studies are imperative to delve into the intricate interplay between microscopic colitis and cardiovascular outcomes, as well as to devise prospective risk prediction methodologies.
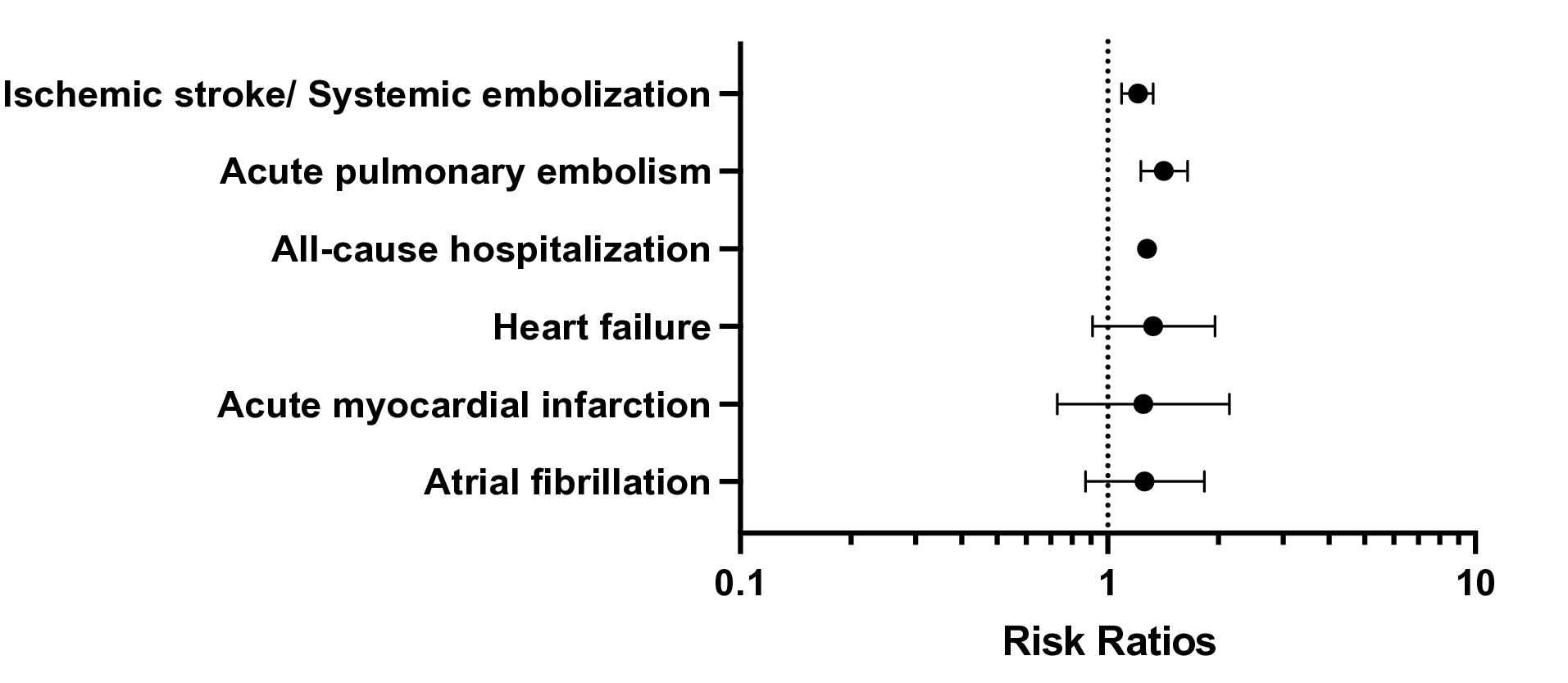
Figure: Figure.1 Coefficient Plot of Cardiovascular Outcomes in Patients with Microscopic Colitis
Disclosures:
Jordan Carty indicated no relevant financial relationships.
Phuuwadith Wattanachayakul indicated no relevant financial relationships.
Evan Isaacs indicated no relevant financial relationships.
Oluwanifemi Balogun indicated no relevant financial relationships.
Jessica Genkil indicated no relevant financial relationships.
Tinsae Anebo indicated no relevant financial relationships.
Karecia Byfield indicated no relevant financial relationships.
Sahana Tito indicated no relevant financial relationships.
Colton Jones indicated no relevant financial relationships.
Carlo Gabriel Casipit indicated no relevant financial relationships.
Michael Goldberg indicated no relevant financial relationships.
Jordan Carty, MD1, Phuuwadith Wattanachayakul, MD1, Evan Isaacs, DO2, Oluwanifemi Balogun, MD1, Jessica Genkil, DO3, Tinsae Anebo, MD1, Karecia Byfield, MBBS1, Sahana Tito, MD4, Colton F. Jones, MBBS1, Carlo Gabriel C. Casipit, MD1, Michael Goldberg, DO1. P4298 - Long-Term Cardiovascular Outcomes Among Patients With Microscopic Colitis: A Propensity Score Matched Analysis from Global Federated Health Research Network, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
