Tuesday Poster Session
Category: IBD
P4303 - Risk of Hypertensive Disorders of Pregnancy in Inflammatory Bowel Disease
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Lindsay Clarke, MD
Brigham and Women's Hospital, Harvard Medical School
Boston, MA
Presenting Author(s)
Award: Presidential Poster Award
Lindsay Clarke, MD1, Sarah Hsu, MS2, Deepti Pant, MPH3, Kaitlyn James, PhD4, Tanayott Thaweethai, PhD5, Lydia L.. Shook, MD4, Jessica R. Allegretti, MD, MPH, FACG6, Rachel W.. Winter, MD, MPH7, Camille Powe, MD4
1Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 2Clinical and Translational Epidemiology Unit, Massachusetts General Hospital, Boston, MA; 3Biostatistics Center, Massachusetts General Hospital, Boston, MA; 4Massachusetts General Hospital, Harvard Medical School, Boston, MA; 5Biostatistics Center, Massachusetts General Hospital; Harvard Medical School, Somerville, MA; 6Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; 7Brigham and Women's Hospital, Harvard Medical School, Chestnut Hill, MA
Introduction: Inflammatory Bowel Disease (IBD), including Crohn’s Disease (CD) and Ulcerative Colitis (UC), is prevalent during reproductive years, and active disease has been associated with adverse pregnancy outcomes. Given prior limited data, we aim to test the hypothesis that IBD is associated with an increased risk of hypertensive disorders of pregnancy (HDP).
Methods: We performed a retrospective cohort electronic health record-based study of singleton pregnancies that delivered at >24 weeks’ gestation between 1998 and 2016 at an academic medical center. IBD was defined using a validated algorithm with diagnosis codes and problem list terms for CD or UC. The primary outcome was pregnancy-specific HDP (gestational hypertension or preeclampsia), defined using a validated algorithm based on American College of Obstetrics and Gynecology criteria. Secondary outcomes include preeclampsia, gestational hypertension, gestational diabetes, preterm delivery, severe perineal lacerations, and small/large for gestational age birthweight (SGA/LGA). Generalized estimated equations were used to determine the association of IBD with outcomes, with adjustment for maternal age at delivery, body mass index (BMI) and systolic BP at 12 weeks’ gestation, insurance, race, and parity.
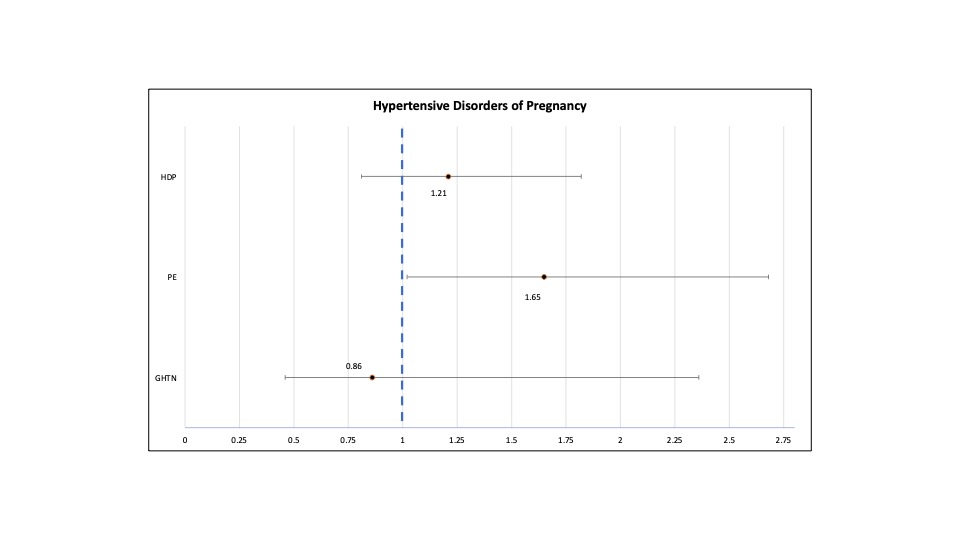
Results: A total of 402 pregnancies (293 individuals) with IBD and 51,926 pregnancies (36,562 individuals) without IBD were included. Patients with IBD were older (32.76±4.57 vs 30.91±5.85 years, P< 0.001), had higher first trimester systolic BP (109.0±8.04 vs 107.75±8.86 mmHg, P=0.005), and lower BMI (24.86±5.21 vs 25.51±5.32 (kg/m2), P=0.015) than those without IBD. Patients with IBD were more likely to be White (90.31% vs 58.38%, P< 0.001) and to have private insurance (81.09 vs 63.81, P< 0.001). There was no association of HDP overall with IBD compared to without (OR 1.21 95% CI [0.81, 1.82], P=0.35). When HDP was sub-categorized, IBD was associated with an increased odds of preeclampsia (OR 1.65 [95% CI 1.02, 2.68], P=0.04), but not gestational hypertension (OR 0.86 [95% CI 0.46, 1.63], P=0.66). There was an association between IBD and preterm delivery (OR 1.67, [95% CI 1.18, 2.37], P=0.004), and SGA (OR 1.68 [95% CI 1.19, 2.39)]), but not other secondary outcomes.
Discussion: Pregnant individuals with IBD have an increased risk of preeclampsia, preterm delivery, and SGA, which potentially reflect underlying placental dysfunction.
Disclosures:
Lindsay Clarke, MD1, Sarah Hsu, MS2, Deepti Pant, MPH3, Kaitlyn James, PhD4, Tanayott Thaweethai, PhD5, Lydia L.. Shook, MD4, Jessica R. Allegretti, MD, MPH, FACG6, Rachel W.. Winter, MD, MPH7, Camille Powe, MD4. P4303 - Risk of Hypertensive Disorders of Pregnancy in Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Lindsay Clarke, MD1, Sarah Hsu, MS2, Deepti Pant, MPH3, Kaitlyn James, PhD4, Tanayott Thaweethai, PhD5, Lydia L.. Shook, MD4, Jessica R. Allegretti, MD, MPH, FACG6, Rachel W.. Winter, MD, MPH7, Camille Powe, MD4
1Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 2Clinical and Translational Epidemiology Unit, Massachusetts General Hospital, Boston, MA; 3Biostatistics Center, Massachusetts General Hospital, Boston, MA; 4Massachusetts General Hospital, Harvard Medical School, Boston, MA; 5Biostatistics Center, Massachusetts General Hospital; Harvard Medical School, Somerville, MA; 6Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; 7Brigham and Women's Hospital, Harvard Medical School, Chestnut Hill, MA
Introduction: Inflammatory Bowel Disease (IBD), including Crohn’s Disease (CD) and Ulcerative Colitis (UC), is prevalent during reproductive years, and active disease has been associated with adverse pregnancy outcomes. Given prior limited data, we aim to test the hypothesis that IBD is associated with an increased risk of hypertensive disorders of pregnancy (HDP).
Methods: We performed a retrospective cohort electronic health record-based study of singleton pregnancies that delivered at >24 weeks’ gestation between 1998 and 2016 at an academic medical center. IBD was defined using a validated algorithm with diagnosis codes and problem list terms for CD or UC. The primary outcome was pregnancy-specific HDP (gestational hypertension or preeclampsia), defined using a validated algorithm based on American College of Obstetrics and Gynecology criteria. Secondary outcomes include preeclampsia, gestational hypertension, gestational diabetes, preterm delivery, severe perineal lacerations, and small/large for gestational age birthweight (SGA/LGA). Generalized estimated equations were used to determine the association of IBD with outcomes, with adjustment for maternal age at delivery, body mass index (BMI) and systolic BP at 12 weeks’ gestation, insurance, race, and parity.
Results: A total of 402 pregnancies (293 individuals) with IBD and 51,926 pregnancies (36,562 individuals) without IBD were included. Patients with IBD were older (32.76±4.57 vs 30.91±5.85 years, P< 0.001), had higher first trimester systolic BP (109.0±8.04 vs 107.75±8.86 mmHg, P=0.005), and lower BMI (24.86±5.21 vs 25.51±5.32 (kg/m2), P=0.015) than those without IBD. Patients with IBD were more likely to be White (90.31% vs 58.38%, P< 0.001) and to have private insurance (81.09 vs 63.81, P< 0.001). There was no association of HDP overall with IBD compared to without (OR 1.21 95% CI [0.81, 1.82], P=0.35). When HDP was sub-categorized, IBD was associated with an increased odds of preeclampsia (OR 1.65 [95% CI 1.02, 2.68], P=0.04), but not gestational hypertension (OR 0.86 [95% CI 0.46, 1.63], P=0.66). There was an association between IBD and preterm delivery (OR 1.67, [95% CI 1.18, 2.37], P=0.004), and SGA (OR 1.68 [95% CI 1.19, 2.39)]), but not other secondary outcomes.
Discussion: Pregnant individuals with IBD have an increased risk of preeclampsia, preterm delivery, and SGA, which potentially reflect underlying placental dysfunction.
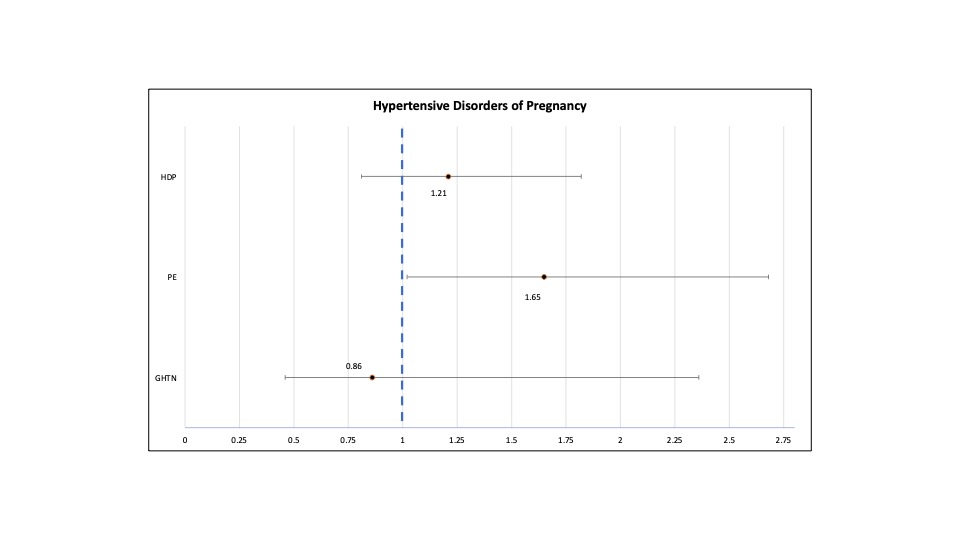
Figure: The adjusted odds of hypertensive disorders of pregnancy (HDP), preeclampsia (PE), and gestational hypertension (GHTN) in IBD.
Disclosures:
Lindsay Clarke indicated no relevant financial relationships.
Sarah Hsu indicated no relevant financial relationships.
Deepti Pant indicated no relevant financial relationships.
Kaitlyn James indicated no relevant financial relationships.
Tanayott Thaweethai indicated no relevant financial relationships.
Lydia Shook: Dexcom – Grant/Research Support. UpToDate – Royalties.
Jessica R. Allegretti: Abbvie – Consultant, Speakers Bureau. Artugen – Consultant. Bristol Myers Squibb – Consultant, Speakers Bureau. Ferring – Consultant. Finch Therapeutics – Consultant. Janssen – Consultant. Merck – Grant/Research Support. Pfizer – Consultant. Seres – Consultant.
Rachel Winter: AbbVie – Consultant, Grant/Research Support. Bristol Myers Squibb – Consultant. Janssen – Grant/Research Support. Takeda – Grant/Research Support.
Camille Powe indicated no relevant financial relationships.
Lindsay Clarke, MD1, Sarah Hsu, MS2, Deepti Pant, MPH3, Kaitlyn James, PhD4, Tanayott Thaweethai, PhD5, Lydia L.. Shook, MD4, Jessica R. Allegretti, MD, MPH, FACG6, Rachel W.. Winter, MD, MPH7, Camille Powe, MD4. P4303 - Risk of Hypertensive Disorders of Pregnancy in Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

