Tuesday Poster Session
Category: IBD
P4304 - Safety and Effectiveness of Glucagon-Like Peptide 1 Receptor Agonists for Obesity in Patients With Inflammatory Bowel Disease
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Lindsay Clarke, MD
Brigham and Women's Hospital, Harvard Medical School
Boston, MA
Presenting Author(s)
Lindsay Clarke, MD1, Ravi Teja Pasam, MBBS, MPH2, Pichamol Jirapinyo, MD, MPH3, Jessica R. Allegretti, MD, MPH, FACG4, Colleen R. Kelly, MD, FACG5
1Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 2Mass General Brigham, Boston, MA; 3Brigham and Women's Hospital, Boston, MA; 4Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; 5Brigham and Women's Hospital, Harvard Medical School, Boston, MA
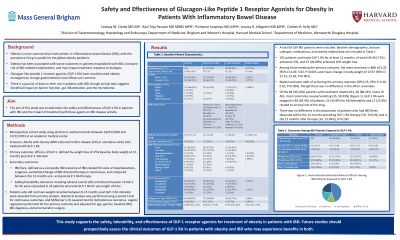
Introduction: Obesity is common in inflammatory bowel disease (IBD) and has a negative impact on disease outcomes. Glucagon-like peptide 1 receptor agonists (GLP-1 RA) have revolutionized obesity management, though GI effects are common. There is little data on use in patients with IBD, though studies suggest beneficial impact on barrier function, inflammation, and the microbiome. We aimed to determine the safety, effectiveness, and impact on IBD disease activity of GLP-1 RA in patients with IBD.
Methods: This is a retrospective cohort study of adults with obesity (BMI ≥30) and IBD treated with GLP-1 RA between 01/01/2020 and 12/31/2023 at an academic medical center. The primary outcome was effectiveness of GLP-1, defined by weight loss of ≥5% baseline body weight at 12-months post GLP-1RA initiation. IBD flare was defined as a composite outcome (IBD-related ED visits or hospitalizations, surgeries, escalation/change of IBD-directed therapy or steroid use) and compared between the 12-months pre- and post-GLP-1 RA. Safety outcomes were calculated in all patients who took GLP-1 RA for any duration. Patients without weight recorded post GLP-1 RA were excluded from primary analysis. Statistical analysis was performed using a paired t-test for continuous outcomes, and McNemar’s chi squared test for dichotomous outcomes. Logistic regression was performed for the primary outcome and adjusted for age, gender, baseline BMI, IBD diagnosis, and prior bariatric surgery.
Results: A total of169 patients were included (Table 1). Of 102 patients on GLP-1 RA for at least 12 months, 66 (64.7%) achieved ³5% and 47 (46.1%) achieved ³10% weight loss, with a mean decrease in BMI was 5.20 (95% CI 4.49, 5.92, P< 0.001) and mean change in body weight of 13.97kg (95% CI 12.32, 15.62, P< 0.001). Males had lower odds of achieving the primary outcome (OR 0.25, 95% CI 0.10, 0.62, P=0.003), with no difference in the other covariates. Of the 68 (40.2%) patients with treatment related AEs, 60 (88.2%) were GI, most commonly nausea/vomiting (35, 58.3%). GLP-1 RA were stopped in 48 (28.4%) of patients; 22 (45.8%) for AE/tolerability and 11 (22.9%) for drug access/cost. There was no difference in IBD flares observed within the 12 months preceding GLP-1 RA therapy (20, 19.6%) vs the 12 months after (16, 15.7%), (P=0.54).
Discussion: This study supports the safety, tolerability, and effectiveness of GLP-1RA for treatment of obesity in patients with IBD. Prospective clinical trials are needed given the potential for benefit in both diseases.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Lindsay Clarke, MD1, Ravi Teja Pasam, MBBS, MPH2, Pichamol Jirapinyo, MD, MPH3, Jessica R. Allegretti, MD, MPH, FACG4, Colleen R. Kelly, MD, FACG5. P4304 - Safety and Effectiveness of Glucagon-Like Peptide 1 Receptor Agonists for Obesity in Patients With Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 2Mass General Brigham, Boston, MA; 3Brigham and Women's Hospital, Boston, MA; 4Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; 5Brigham and Women's Hospital, Harvard Medical School, Boston, MA
Introduction: Obesity is common in inflammatory bowel disease (IBD) and has a negative impact on disease outcomes. Glucagon-like peptide 1 receptor agonists (GLP-1 RA) have revolutionized obesity management, though GI effects are common. There is little data on use in patients with IBD, though studies suggest beneficial impact on barrier function, inflammation, and the microbiome. We aimed to determine the safety, effectiveness, and impact on IBD disease activity of GLP-1 RA in patients with IBD.
Methods: This is a retrospective cohort study of adults with obesity (BMI ≥30) and IBD treated with GLP-1 RA between 01/01/2020 and 12/31/2023 at an academic medical center. The primary outcome was effectiveness of GLP-1, defined by weight loss of ≥5% baseline body weight at 12-months post GLP-1RA initiation. IBD flare was defined as a composite outcome (IBD-related ED visits or hospitalizations, surgeries, escalation/change of IBD-directed therapy or steroid use) and compared between the 12-months pre- and post-GLP-1 RA. Safety outcomes were calculated in all patients who took GLP-1 RA for any duration. Patients without weight recorded post GLP-1 RA were excluded from primary analysis. Statistical analysis was performed using a paired t-test for continuous outcomes, and McNemar’s chi squared test for dichotomous outcomes. Logistic regression was performed for the primary outcome and adjusted for age, gender, baseline BMI, IBD diagnosis, and prior bariatric surgery.
Results: A total of169 patients were included (Table 1). Of 102 patients on GLP-1 RA for at least 12 months, 66 (64.7%) achieved ³5% and 47 (46.1%) achieved ³10% weight loss, with a mean decrease in BMI was 5.20 (95% CI 4.49, 5.92, P< 0.001) and mean change in body weight of 13.97kg (95% CI 12.32, 15.62, P< 0.001). Males had lower odds of achieving the primary outcome (OR 0.25, 95% CI 0.10, 0.62, P=0.003), with no difference in the other covariates. Of the 68 (40.2%) patients with treatment related AEs, 60 (88.2%) were GI, most commonly nausea/vomiting (35, 58.3%). GLP-1 RA were stopped in 48 (28.4%) of patients; 22 (45.8%) for AE/tolerability and 11 (22.9%) for drug access/cost. There was no difference in IBD flares observed within the 12 months preceding GLP-1 RA therapy (20, 19.6%) vs the 12 months after (16, 15.7%), (P=0.54).
Discussion: This study supports the safety, tolerability, and effectiveness of GLP-1RA for treatment of obesity in patients with IBD. Prospective clinical trials are needed given the potential for benefit in both diseases.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Lindsay Clarke indicated no relevant financial relationships.
Ravi Teja Pasam indicated no relevant financial relationships.
Pichamol Jirapinyo: Apollo Endosurgery – Consultant, Grant/Research Support. Bariendo – Advisory Committee/Board Member, Consultant, Owner/Ownership Interest. Boston Scientific – Consultant, Grant/Research Support. Cook Medical – Consultant. Endosim – Royalties. ERBE – Consultant. Fractyl – Consultant, Grant/Research Support. GI Dynamics – Consultant, Grant/Research Support. Madrigal – Consultant. Spatz – Consultant. USGI Medical – Consultant, Grant/Research Support.
Jessica R. Allegretti: Abbvie – Consultant, Speakers Bureau. Artugen – Consultant. Bristol Myers Squibb – Consultant, Speakers Bureau. Ferring – Consultant. Finch Therapeutics – Consultant. Janssen – Consultant. Merck – Grant/Research Support. Pfizer – Consultant. Seres – Consultant.
Colleen Kelly indicated no relevant financial relationships.
Lindsay Clarke, MD1, Ravi Teja Pasam, MBBS, MPH2, Pichamol Jirapinyo, MD, MPH3, Jessica R. Allegretti, MD, MPH, FACG4, Colleen R. Kelly, MD, FACG5. P4304 - Safety and Effectiveness of Glucagon-Like Peptide 1 Receptor Agonists for Obesity in Patients With Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
