Tuesday Poster Session
Category: IBD
P4308 - Improving Sleep Health in Adults With Inflammatory Bowel Disease: A Call for Action
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
- ME
Mohamad Elgozair, MD
Mayo Clinic
Rochester, MN
Presenting Author(s)
Mohamad Elgozair, MD1, Stacy Al-Saleh, RN, PhD1, Melanie Schneekloth, BS1, Sunanda V. Kane, MD, MSPH1, Nancy Redeker, RN, PhD2, Samantha Conley, RN, PhD1
1Mayo Clinic, Rochester, MN; 2University of Connecticut, Storrs, CT
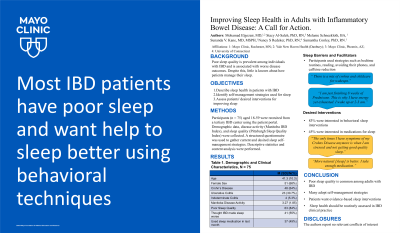
Introduction: Poor sleep quality is highly prevalent among individuals with inflammatory bowel disease (IBD) and is associated with worse IBD outcomes. This issue is multifactorial, but little is known about how patients with IBD manage sleep. The aim of this study was to describe current and desired sleep self-management strategies among adults with IBD.
Methods: In this IRB approved study, adults aged 18 to 59 with IBD were recruited from a single tertiary care IBD center via the patient portal starting in December 2022. We collected demographic characteristics, clinical disease activity (Manitoba IBD Index: active disease = symptoms from constant to occasionally active), and Pittsburgh Sleep Quality Index ( > 5 is poor sleep). Participants' current and desired self-management sleep strategies were elicited using a structured questionnaire supplemented by an open-ended question. We then performed descriptive statistical and content analysis.
Results: Among 75 adults with IBD [Mean age = 41.3 years (SD = 10.3), 51 (68%) female, and 72 (96%) white], most participants had Crohn’s disease (N = 48, 64%). Most surveyed patients (68%, N=51) had active disease. Poor sleep health was highly prevalent in our sample (N = 63, 84%), without a statistically significant difference between those with poor/good sleep health and active/inactive disease (p =0.32). Over half (N= 41, 55%) believed IBD worsened their sleep, and nearly half reported taking over the counter or prescription sleep medication within the last month (N = 37, 49% Participants used bedtime routines, reading, caffeine reduction, and exercise to help them sleep. A quarter of participants (N = 18, 24%) reported that they had never been asked about their sleep by a healthcare provider. The majority of subjects (N = 62, 83%) were interested in behavioral sleep interventions with components that included relaxation (N = 61, 81%), mindfulness (N = 58, 77%), and music (N = 53, 71%). Participants preferred receiving interventions one-on-one (N = 60, 80%) or via an app/website (N = 57, 76%). Nearly half (N = 34, 45%) were interested in sleep medications.
Discussion: Poor sleep quality is highly prevalent in adults with IBD who adopt various self-management sleep strategies. These results highlight the need to develop and test evidence-based sleep health interventions for IBD patients. Sleep quality should be part of an assessment of health in IBD patients, along with resources for improvement.
Disclosures:
Mohamad Elgozair, MD1, Stacy Al-Saleh, RN, PhD1, Melanie Schneekloth, BS1, Sunanda V. Kane, MD, MSPH1, Nancy Redeker, RN, PhD2, Samantha Conley, RN, PhD1. P4308 - Improving Sleep Health in Adults With Inflammatory Bowel Disease: A Call for Action, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic, Rochester, MN; 2University of Connecticut, Storrs, CT
Introduction: Poor sleep quality is highly prevalent among individuals with inflammatory bowel disease (IBD) and is associated with worse IBD outcomes. This issue is multifactorial, but little is known about how patients with IBD manage sleep. The aim of this study was to describe current and desired sleep self-management strategies among adults with IBD.
Methods: In this IRB approved study, adults aged 18 to 59 with IBD were recruited from a single tertiary care IBD center via the patient portal starting in December 2022. We collected demographic characteristics, clinical disease activity (Manitoba IBD Index: active disease = symptoms from constant to occasionally active), and Pittsburgh Sleep Quality Index ( > 5 is poor sleep). Participants' current and desired self-management sleep strategies were elicited using a structured questionnaire supplemented by an open-ended question. We then performed descriptive statistical and content analysis.
Results: Among 75 adults with IBD [Mean age = 41.3 years (SD = 10.3), 51 (68%) female, and 72 (96%) white], most participants had Crohn’s disease (N = 48, 64%). Most surveyed patients (68%, N=51) had active disease. Poor sleep health was highly prevalent in our sample (N = 63, 84%), without a statistically significant difference between those with poor/good sleep health and active/inactive disease (p =0.32). Over half (N= 41, 55%) believed IBD worsened their sleep, and nearly half reported taking over the counter or prescription sleep medication within the last month (N = 37, 49% Participants used bedtime routines, reading, caffeine reduction, and exercise to help them sleep. A quarter of participants (N = 18, 24%) reported that they had never been asked about their sleep by a healthcare provider. The majority of subjects (N = 62, 83%) were interested in behavioral sleep interventions with components that included relaxation (N = 61, 81%), mindfulness (N = 58, 77%), and music (N = 53, 71%). Participants preferred receiving interventions one-on-one (N = 60, 80%) or via an app/website (N = 57, 76%). Nearly half (N = 34, 45%) were interested in sleep medications.
Discussion: Poor sleep quality is highly prevalent in adults with IBD who adopt various self-management sleep strategies. These results highlight the need to develop and test evidence-based sleep health interventions for IBD patients. Sleep quality should be part of an assessment of health in IBD patients, along with resources for improvement.
Disclosures:
Mohamad Elgozair indicated no relevant financial relationships.
Stacy Al-Saleh indicated no relevant financial relationships.
Melanie Schneekloth indicated no relevant financial relationships.
Sunanda Kane: Janssen – Advisory Committee/Board Member.
Nancy Redeker indicated no relevant financial relationships.
Samantha Conley indicated no relevant financial relationships.
Mohamad Elgozair, MD1, Stacy Al-Saleh, RN, PhD1, Melanie Schneekloth, BS1, Sunanda V. Kane, MD, MSPH1, Nancy Redeker, RN, PhD2, Samantha Conley, RN, PhD1. P4308 - Improving Sleep Health in Adults With Inflammatory Bowel Disease: A Call for Action, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
