Tuesday Poster Session
Category: IBD
P4311 - The Natural History of Dysplasia in Inflammatory Bowel Disease: Results of a Markov Model
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Kate E. Lee, MD, MS
Duke University Medical Center
Durham, NC
Presenting Author(s)
Kate E. Lee, MD, MS1, Alice A. Agyekum, BS2, Jane E. Onken, MD, MHS1, Bo Shen, MD3, Francesca Lim, MS2, Jordan Axelrad, MD, MPH4, Aasma Shaukat, MD, MPH5, Chin Hur, MD, MPH2, Adam S.. Faye, MD4
1Duke University Medical Center, Durham, NC; 2Columbia University Irving Medical Center, New York, NY; 3Columbia University, New York, NY; 4NYU Grossman School of Medicine, New York, NY; 5NYU Langone Health, New York, NY
Introduction: Observational studies have suggested that inflammatory bowel disease (IBD) increases the risk of colonic dysplasia. Surveillance colonoscopies can reduce this risk through detection of dysplasia and intervention; however, further research is needed to clarify optimal guidance on interval screening. We therefore aimed to establish a natural history model of dysplasia in IBD assuming no IBD-related surveillance colonoscopies to gain insight into the natural disease course.
Methods: A state-transition Markov model was developed using TreeAge Pro 2024 with a base case of a 30-year-old individual with IBD undergoing their first surveillance (index) colonoscopy 8 years after diagnosis. The initial health-state at index colonoscopy was determined based on published data on the distribution of no dysplasia, low grade dysplasia (LGD), high grade dysplasia (HGD), or colorectal cancer (CRC) at index colonoscopy in the IBD population (Table 1). Individuals could then progress to more advanced states of dysplasia. The cycle length was one year, and patients were followed until death or age 100 years. Cancer incidence and mortality data were obtained from the Surveillance, Epidemiology, and End Results 17 registry. The model was calibrated to incidence data to approximate the probability of developing CRC using DevCan software. We adjusted for an IBD population using a relative risk (2.5) derived from the literature, with outputs providing estimates of dysplasia progression.
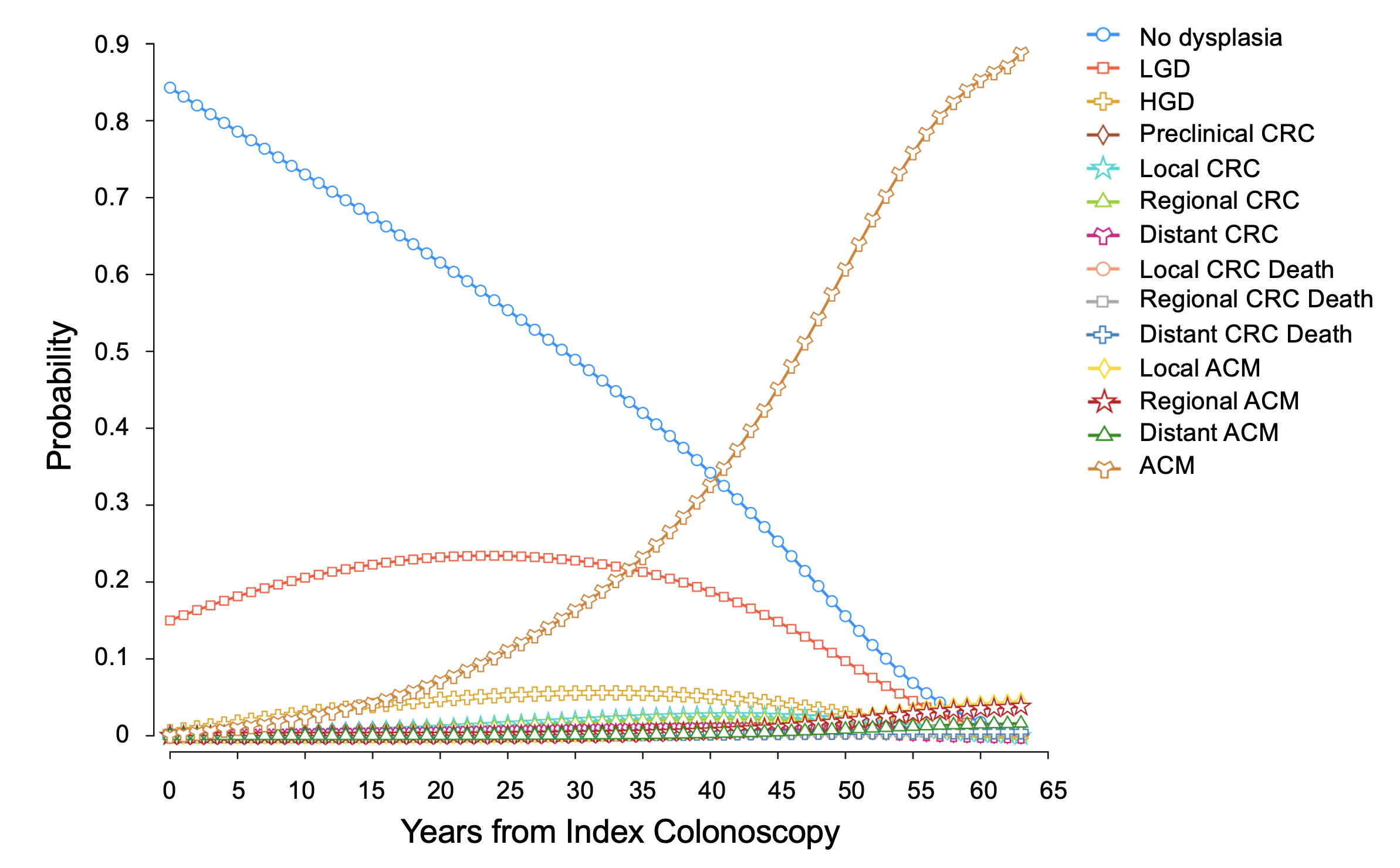
Results: Assuming no IBD-related surveillance colonoscopies (natural history of IBD), the lifetime incidence of CRC in our model was 11.2% (4.8% local, 4.3% regional, 2.1% distant), with 1.2% of patients ultimately dying of CRC itself. Among those who did not have dysplasia on index colonoscopy, an additional 1.2% developed dysplasia one year later, 2.3% at two years, and 3.5% at three years (Table 1). Overall, ten years from index colonoscopy, 20.6% of individuals developed LGD, 2.9% developed HGD, and 0.7% developed CRC; by twenty years from index colonoscopy, 23.2% developed LGD, 4.7% HGD, and 2.4% CRC (Figure 1).
Discussion: Optimal intervals to perform dysplasia screening in IBD remain unknown. Among those with no dysplasia at first surveillance colonoscopy, our model suggests that approximately 1% will develop dysplasia each year (from years 1-3), with approximately 0.7% being LGD. By developing this natural history model, we are now able to model different screening strategies which can help inform future clinical practice.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kate E. Lee, MD, MS1, Alice A. Agyekum, BS2, Jane E. Onken, MD, MHS1, Bo Shen, MD3, Francesca Lim, MS2, Jordan Axelrad, MD, MPH4, Aasma Shaukat, MD, MPH5, Chin Hur, MD, MPH2, Adam S.. Faye, MD4. P4311 - The Natural History of Dysplasia in Inflammatory Bowel Disease: Results of a Markov Model, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Duke University Medical Center, Durham, NC; 2Columbia University Irving Medical Center, New York, NY; 3Columbia University, New York, NY; 4NYU Grossman School of Medicine, New York, NY; 5NYU Langone Health, New York, NY
Introduction: Observational studies have suggested that inflammatory bowel disease (IBD) increases the risk of colonic dysplasia. Surveillance colonoscopies can reduce this risk through detection of dysplasia and intervention; however, further research is needed to clarify optimal guidance on interval screening. We therefore aimed to establish a natural history model of dysplasia in IBD assuming no IBD-related surveillance colonoscopies to gain insight into the natural disease course.
Methods: A state-transition Markov model was developed using TreeAge Pro 2024 with a base case of a 30-year-old individual with IBD undergoing their first surveillance (index) colonoscopy 8 years after diagnosis. The initial health-state at index colonoscopy was determined based on published data on the distribution of no dysplasia, low grade dysplasia (LGD), high grade dysplasia (HGD), or colorectal cancer (CRC) at index colonoscopy in the IBD population (Table 1). Individuals could then progress to more advanced states of dysplasia. The cycle length was one year, and patients were followed until death or age 100 years. Cancer incidence and mortality data were obtained from the Surveillance, Epidemiology, and End Results 17 registry. The model was calibrated to incidence data to approximate the probability of developing CRC using DevCan software. We adjusted for an IBD population using a relative risk (2.5) derived from the literature, with outputs providing estimates of dysplasia progression.
Results: Assuming no IBD-related surveillance colonoscopies (natural history of IBD), the lifetime incidence of CRC in our model was 11.2% (4.8% local, 4.3% regional, 2.1% distant), with 1.2% of patients ultimately dying of CRC itself. Among those who did not have dysplasia on index colonoscopy, an additional 1.2% developed dysplasia one year later, 2.3% at two years, and 3.5% at three years (Table 1). Overall, ten years from index colonoscopy, 20.6% of individuals developed LGD, 2.9% developed HGD, and 0.7% developed CRC; by twenty years from index colonoscopy, 23.2% developed LGD, 4.7% HGD, and 2.4% CRC (Figure 1).
Discussion: Optimal intervals to perform dysplasia screening in IBD remain unknown. Among those with no dysplasia at first surveillance colonoscopy, our model suggests that approximately 1% will develop dysplasia each year (from years 1-3), with approximately 0.7% being LGD. By developing this natural history model, we are now able to model different screening strategies which can help inform future clinical practice.
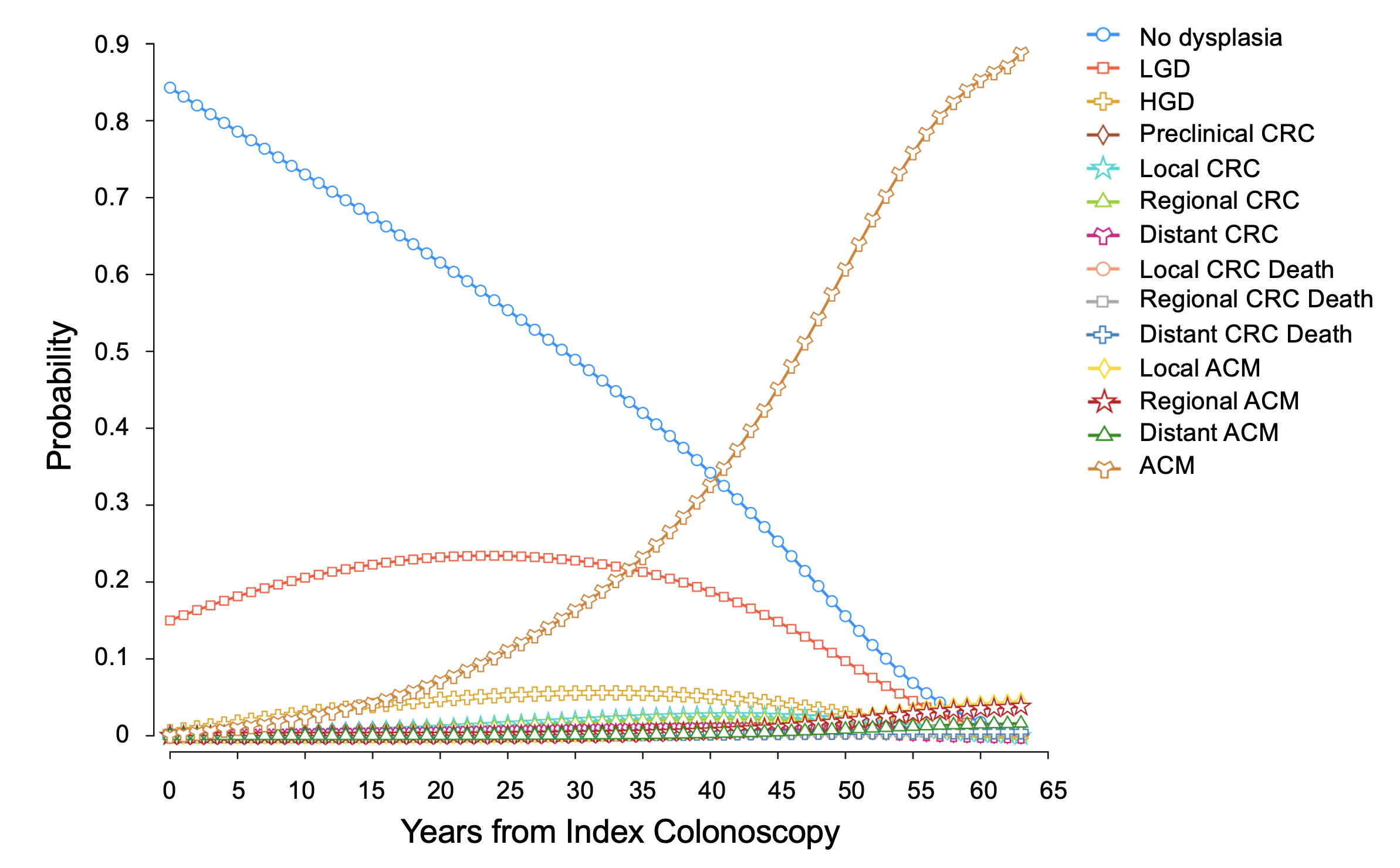
Figure: Figure 1. Dysplasia evolution by year from index colonoscopy.
Index colonoscopy is performed at age 38 in the model assuming 8 years after age of diagnosis of 30 years. Hence, year 62 corresponds to age 100.
Abbreviations: ACM (all cause mortality), CRC (colorectal cancer), HGD (high grade dysplasia), LGD (low grade dysplasia).
Index colonoscopy is performed at age 38 in the model assuming 8 years after age of diagnosis of 30 years. Hence, year 62 corresponds to age 100.
Abbreviations: ACM (all cause mortality), CRC (colorectal cancer), HGD (high grade dysplasia), LGD (low grade dysplasia).
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kate Lee indicated no relevant financial relationships.
Alice Agyekum indicated no relevant financial relationships.
Jane Onken indicated no relevant financial relationships.
Bo Shen indicated no relevant financial relationships.
Francesca Lim indicated no relevant financial relationships.
Jordan Axelrad: Abbvie – Consultant. Adiso – Consultant. Biomerieux – Consultant. BMS – Consultant. Fresenius – Consultant. Genentech – Grant/Research Support. Janssen – Consultant. Pfizer – Consultant.
Aasma Shaukat: iterative health; Freenome – Consultant.
Chin Hur indicated no relevant financial relationships.
Adam Faye: Abbvie – Consultant. BMS – Consultant. Takeda – Education Seminar.
Kate E. Lee, MD, MS1, Alice A. Agyekum, BS2, Jane E. Onken, MD, MHS1, Bo Shen, MD3, Francesca Lim, MS2, Jordan Axelrad, MD, MPH4, Aasma Shaukat, MD, MPH5, Chin Hur, MD, MPH2, Adam S.. Faye, MD4. P4311 - The Natural History of Dysplasia in Inflammatory Bowel Disease: Results of a Markov Model, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

