Tuesday Poster Session
Category: IBD
P4326 - Demographics, Complications, and Healthcare Utilization of Ethnically Hispanic vs Non-Hispanic Patients with Inflammatory Bowel Disease
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- GD
Gerardo Diaz Garcia, DO
University of Florida College of Medicine
Jacksonville, FL
Presenting Author(s)
Gerardo Diaz Garcia, DO1, Landen Shane Burstiner, DO, MSc1, Oshin Rai, DO1, Anvit Reddy, DO1, Nadim A. Qadir, DO2, Tara Kronen, DO, MA1, Luke Stachler, MD1, Marianny Sulbaran Nava, MD, PhD, MS1, Lauren N.. Stemboroski, DO1
1University of Florida College of Medicine, Jacksonville, FL; 2University of Florida College of Medicine, Windermere, FL
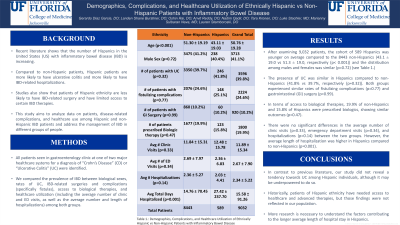
Introduction: Recent literature shows that the number of Hispanics in the United States (US) with inflammatory bowel disease (IBD) is increasing. Compared to non-Hispanic patients, Hispanic patients are more likely to have ulcerative colitis and more likely to have IBD-related hospitalizations. Studies also show that patients of Hispanic ethnicity are less likely to have IBD-related surgery and have limited access to certain IBD therapies. This study aims to analyze data on patients, disease-related complications, and healthcare use among Hispanic and non-Hispanic IBD patients and address the management of IBD in different groups of people.
Methods: All patients seen in gastroenterology clinic at one of two major healthcare systems for a diagnosis of “Crohn’s Disease” (CD) or “Ulcerative Colitis” (UC) were identified. We compared the prevalence of IBD between biological sexes, rates of UC, IBD-related surgeries and complications (specifically fistulas), access to biological therapies, and healthcare utilization (including the average number of clinic and ED visits, as well as the average number and length of hospitalizations) among both groups.
Results: After examining 9,032 patients, the cohort of 589 Hispanics was younger on average compared to the 8443 non-Hispanics (43.1 ± 19.0 vs 51.3 ± 19.0, respectively (p< 0.001)) and the distribution among males and females was similar (p=0.72) (see Table 1.). The presence of UC was similar in Hispanics compared to non-Hispanics (41.8% vs 39.7%, respectively (p=0.32)). Both groups experienced similar rates of fistulizing complications (p=0.77) and gastrointestinal (GI) surgery (p=0.99). In terms of access to biological therapies, 19.9% of non-Hispanics and 15.8% of Hispanics were prescribed biologics, showing similar outcomes (p=0.47). There were no significant differences in the average number of clinic visits (p=0.33), emergency department visits (p=0.34), and hospitalizations (p=0.14) between the two groups. However, the average length of hospitalization was higher in Hispanics compared to non-Hispanics (p=0.001).
Discussion: In contrast to previous literature, our study did not reveal a tendency towards UC among Hispanic individuals, although it may be underpowered to do so. Historically, patients of Hispanic ethnicity have needed access to healthcare and advanced therapies, but those findings were not reflected in our population. More research is necessary to understand the factors contributing to the longer average length of hospital stay in Hispanics.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Gerardo Diaz Garcia, DO1, Landen Shane Burstiner, DO, MSc1, Oshin Rai, DO1, Anvit Reddy, DO1, Nadim A. Qadir, DO2, Tara Kronen, DO, MA1, Luke Stachler, MD1, Marianny Sulbaran Nava, MD, PhD, MS1, Lauren N.. Stemboroski, DO1. P4326 - Demographics, Complications, and Healthcare Utilization of Ethnically Hispanic vs Non-Hispanic Patients with Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Florida College of Medicine, Jacksonville, FL; 2University of Florida College of Medicine, Windermere, FL
Introduction: Recent literature shows that the number of Hispanics in the United States (US) with inflammatory bowel disease (IBD) is increasing. Compared to non-Hispanic patients, Hispanic patients are more likely to have ulcerative colitis and more likely to have IBD-related hospitalizations. Studies also show that patients of Hispanic ethnicity are less likely to have IBD-related surgery and have limited access to certain IBD therapies. This study aims to analyze data on patients, disease-related complications, and healthcare use among Hispanic and non-Hispanic IBD patients and address the management of IBD in different groups of people.
Methods: All patients seen in gastroenterology clinic at one of two major healthcare systems for a diagnosis of “Crohn’s Disease” (CD) or “Ulcerative Colitis” (UC) were identified. We compared the prevalence of IBD between biological sexes, rates of UC, IBD-related surgeries and complications (specifically fistulas), access to biological therapies, and healthcare utilization (including the average number of clinic and ED visits, as well as the average number and length of hospitalizations) among both groups.
Results: After examining 9,032 patients, the cohort of 589 Hispanics was younger on average compared to the 8443 non-Hispanics (43.1 ± 19.0 vs 51.3 ± 19.0, respectively (p< 0.001)) and the distribution among males and females was similar (p=0.72) (see Table 1.). The presence of UC was similar in Hispanics compared to non-Hispanics (41.8% vs 39.7%, respectively (p=0.32)). Both groups experienced similar rates of fistulizing complications (p=0.77) and gastrointestinal (GI) surgery (p=0.99). In terms of access to biological therapies, 19.9% of non-Hispanics and 15.8% of Hispanics were prescribed biologics, showing similar outcomes (p=0.47). There were no significant differences in the average number of clinic visits (p=0.33), emergency department visits (p=0.34), and hospitalizations (p=0.14) between the two groups. However, the average length of hospitalization was higher in Hispanics compared to non-Hispanics (p=0.001).
Discussion: In contrast to previous literature, our study did not reveal a tendency towards UC among Hispanic individuals, although it may be underpowered to do so. Historically, patients of Hispanic ethnicity have needed access to healthcare and advanced therapies, but those findings were not reflected in our population. More research is necessary to understand the factors contributing to the longer average length of hospital stay in Hispanics.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Gerardo Diaz Garcia indicated no relevant financial relationships.
Landen Shane Burstiner indicated no relevant financial relationships.
Oshin Rai indicated no relevant financial relationships.
Anvit Reddy indicated no relevant financial relationships.
Nadim Qadir indicated no relevant financial relationships.
Tara Kronen indicated no relevant financial relationships.
Luke Stachler indicated no relevant financial relationships.
Marianny Sulbaran Nava indicated no relevant financial relationships.
Lauren Stemboroski indicated no relevant financial relationships.
Gerardo Diaz Garcia, DO1, Landen Shane Burstiner, DO, MSc1, Oshin Rai, DO1, Anvit Reddy, DO1, Nadim A. Qadir, DO2, Tara Kronen, DO, MA1, Luke Stachler, MD1, Marianny Sulbaran Nava, MD, PhD, MS1, Lauren N.. Stemboroski, DO1. P4326 - Demographics, Complications, and Healthcare Utilization of Ethnically Hispanic vs Non-Hispanic Patients with Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
