Tuesday Poster Session
Category: IBD
P4367 - Racial Disparities in Venous Thromboembolism Events in Ulcerative Colitis Admissions: A Six-Year US National Experience
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Abhin Sapkota, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Abhin Sapkota, MD1, Bhanu Siva Mohan Pinnam, MD1, Daksh Ahluwalia, MD1, Dushyant S. Dahiya, MD2, Hassam Ali, MD3, Saurabh Chandan, MD4, Seema Gandhi, MD1
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2The University of Kansas School of Medicine, Kansas City, KS; 3East Carolina University, Greenville, NC; 4CHI Health Creighton University Medical Center, Omaha, NE
Introduction: Patients with Ulcerative Colitis (UC) are at a higher risk of developing venous thromboembolism (VTE). Racial differences in various disease outcomes are well-documented in past literature, but there is limited data on the effect of such disparities on the occurrence of VTE in UC. This study aims to explore the impact of race on the incidence of VTE among patients with UC while considering potential confounding demographics.
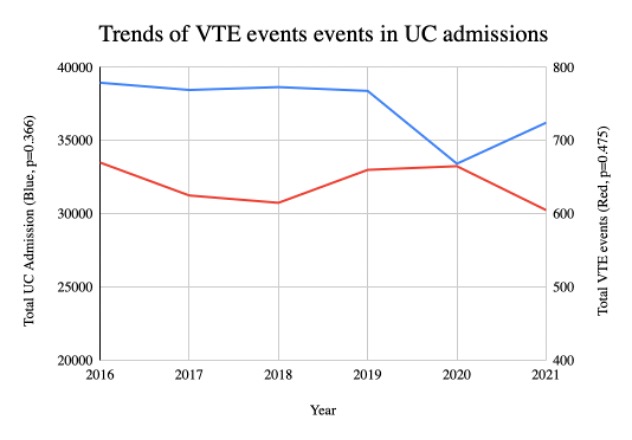
Methods: The National Inpatient Sample 2016 through 2021 was used for this study. We identified all cases with a primary diagnosis of UC using the International Classification of Diseases, 10th revision codes. VTE events included acute deep vein thrombosis of the upper and lower extremities and acute pulmonary embolism as a secondary diagnosis. Hospitalization characteristics were highlighted and compared. A multivariate regression analysis was used to compare independent predictors of VTE events. Trend analysis for UC admissions and VTE events was also done. A P-value of < 0.05 was considered statistically significant.
Results: There were 224,085 UC admissions, among which 3,840 (1.71%) developed VTE events. Patients who had VTE had a higher mean age than those without VTE events (55.88 vs 45.95 years, p< 0.001). Patients with VTE had a significantly longer length of stay (LOS) than those without VTE events (13.82 vs 5.21 days, p=0.037). Black patients had the highest percentage of VTE events (1.65%), followed by white (1.42%), hispanic (1.11%), and other races (1.05%). Compared to Hispanic patients, black patients were at a higher risk of VTE (1.65%. vs. 1.11%, odds ratio (OR) 1.65, p< 0.01), and so were white patients (1.42% vs 1.11%, OR 1.42, p=0.015). A Charlson Comorbidity index (CCI) of 3 or more (OR 1.37, p=0.011) and admission at metropolitan teaching hospitals (OR 2.09, p< 0.001) were also predictors of VTE.
Discussion: This study highlights significant racial disparities in the incidence of VTE in UC. Black and white racial groups were found to be at a higher risk of VTE compared to hispanic patients, suggesting a role of possible underlying genetic, socioeconomic, or healthcare access factors. Patients with VTE events have a longer average LOS and total costs, indicating the healthcare burden of these events. The increased risk associated with higher comorbidity indices and specific hospital types emphasizes the need for more targeted and customized approaches to mitigate VTE risk in these groups. Further research is needed to explore these disparities.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Abhin Sapkota, MD1, Bhanu Siva Mohan Pinnam, MD1, Daksh Ahluwalia, MD1, Dushyant S. Dahiya, MD2, Hassam Ali, MD3, Saurabh Chandan, MD4, Seema Gandhi, MD1. P4367 - Racial Disparities in Venous Thromboembolism Events in Ulcerative Colitis Admissions: A Six-Year US National Experience, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2The University of Kansas School of Medicine, Kansas City, KS; 3East Carolina University, Greenville, NC; 4CHI Health Creighton University Medical Center, Omaha, NE
Introduction: Patients with Ulcerative Colitis (UC) are at a higher risk of developing venous thromboembolism (VTE). Racial differences in various disease outcomes are well-documented in past literature, but there is limited data on the effect of such disparities on the occurrence of VTE in UC. This study aims to explore the impact of race on the incidence of VTE among patients with UC while considering potential confounding demographics.
Methods: The National Inpatient Sample 2016 through 2021 was used for this study. We identified all cases with a primary diagnosis of UC using the International Classification of Diseases, 10th revision codes. VTE events included acute deep vein thrombosis of the upper and lower extremities and acute pulmonary embolism as a secondary diagnosis. Hospitalization characteristics were highlighted and compared. A multivariate regression analysis was used to compare independent predictors of VTE events. Trend analysis for UC admissions and VTE events was also done. A P-value of < 0.05 was considered statistically significant.
Results: There were 224,085 UC admissions, among which 3,840 (1.71%) developed VTE events. Patients who had VTE had a higher mean age than those without VTE events (55.88 vs 45.95 years, p< 0.001). Patients with VTE had a significantly longer length of stay (LOS) than those without VTE events (13.82 vs 5.21 days, p=0.037). Black patients had the highest percentage of VTE events (1.65%), followed by white (1.42%), hispanic (1.11%), and other races (1.05%). Compared to Hispanic patients, black patients were at a higher risk of VTE (1.65%. vs. 1.11%, odds ratio (OR) 1.65, p< 0.01), and so were white patients (1.42% vs 1.11%, OR 1.42, p=0.015). A Charlson Comorbidity index (CCI) of 3 or more (OR 1.37, p=0.011) and admission at metropolitan teaching hospitals (OR 2.09, p< 0.001) were also predictors of VTE.
Discussion: This study highlights significant racial disparities in the incidence of VTE in UC. Black and white racial groups were found to be at a higher risk of VTE compared to hispanic patients, suggesting a role of possible underlying genetic, socioeconomic, or healthcare access factors. Patients with VTE events have a longer average LOS and total costs, indicating the healthcare burden of these events. The increased risk associated with higher comorbidity indices and specific hospital types emphasizes the need for more targeted and customized approaches to mitigate VTE risk in these groups. Further research is needed to explore these disparities.
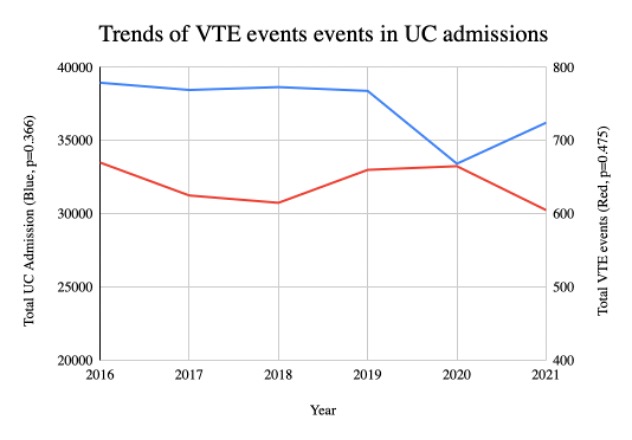
Figure: Trends of Venous Thromboembolism (VTE) events in Ulcerative Colitis (UC) admissions
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Abhin Sapkota indicated no relevant financial relationships.
Bhanu Siva Mohan Pinnam indicated no relevant financial relationships.
Daksh Ahluwalia indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Hassam Ali indicated no relevant financial relationships.
Saurabh Chandan indicated no relevant financial relationships.
Seema Gandhi indicated no relevant financial relationships.
Abhin Sapkota, MD1, Bhanu Siva Mohan Pinnam, MD1, Daksh Ahluwalia, MD1, Dushyant S. Dahiya, MD2, Hassam Ali, MD3, Saurabh Chandan, MD4, Seema Gandhi, MD1. P4367 - Racial Disparities in Venous Thromboembolism Events in Ulcerative Colitis Admissions: A Six-Year US National Experience, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
