Tuesday Poster Session
Category: IBD
P4369 - GLP-1 Agonists are Associated With Lower Rates of IBD-Related Complications in Patients With Elevated BMI Compared to Bariatric Surgery: A Nationwide Cohort Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

M Housam Nanah, MD
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
M Housam Nanah, MD1, Robana Nanah, MD2, Rama Nanah, MD1, Rashid Abdel-Razeq, MD1, Gauri Pikale, MD3, Abdullah Hafeez, MD4, Miguel D Regueiro, MD1
1Cleveland Clinic, Cleveland, OH; 2University of Aleppo, Cleveland, OH; 3Chicago Medical School at Rosalind Franklin University of Medicine and Science, Chicago, IL; 4Landmark Medical Center, Cumberland, RI
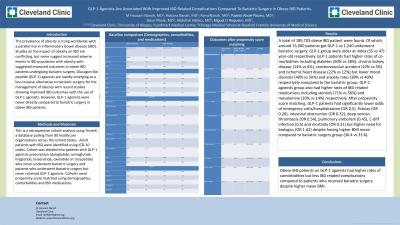
Introduction: The prevalence of obesity is rising worldwide with a parallel rise in inflammatory bowel disease (IBD). Studies on the impact of obesity on IBD are conflicting, but some suggest increased adverse events in IBD population with obesity with suggested improved outcomes in obese IBD patients undergoing bariatric surgery. Glucagon-like peptide (GLP-1) agonists are rapidly emerging as a less invasive alternative to bariatric surgery for the management of obesity with recent studies showing improved IBD outcomes with the use of GLP-1 agonists. However, GLP-1 agonists were never directly compared to bariatric surgery in obese IBD patients.
Methods: This is a retrospective cohort analysis using TrinetX, a database pulling from 80 healthcare organizations across the United States. Adult patients with IBD were identified using ICD-10 codes. Cohort was divided into patients with GLP-1 agonists prescription (dulaglutide, semaglutide, liraglutide, lixisenatide, exenatide or tirzepatide) who never underwent bariatric surgery and patients who underwent bariatric surgery but never received GLP-1 agonists. Cohorts were propensity score matched using demographics, comorbidities and IBD medications.
Results: A total of 189,703 obese IBD patient were found. Of which, around 15,000 patients got GLP-1 vs 1,240 underwent bariatric surgery. GLP-1 group were older at index (55 vs 47) year-old respectively. GLP-1 patients had higher rates of co-morbidities including diabetes (60% vs 28%), chronic kidney disease (14% vs 6%), cerebrovascular accident (10% vs 5%) and ischemic heart disease (22% vs 12%) but lower mood disorder (40% vs 50%) and anxiety rates (38% vs 40%) respectively compared to the bariatric group. GLP-1 agonists group also had higher rates of IBD related medications including steroids (71% vs 56%) and mesalamine (20% vs 14%) respectively. After propensity score matching, GLP-1 patients had significantly lower odds of emergency visits/hospitalization (OR 0.5), fistulas (OR 0.26), intestinal obstruction (OR 0.32), deep venous thrombosis (OR 0.54), pulmonary embolism (0.45), C-diff infection (0.5) and mortality (OR 0.31) but higher need for biologics (OR 1.42) despite having higher BMI mean compared to bariatric surgery group (36.4 vs 33.6).
Discussion: Obese IBD patients on GLP-1 agonists had higher rates of comorbidities but less IBD related complications compared to patients who received bariatric surgery despite higher mean BMI.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
M Housam Nanah, MD1, Robana Nanah, MD2, Rama Nanah, MD1, Rashid Abdel-Razeq, MD1, Gauri Pikale, MD3, Abdullah Hafeez, MD4, Miguel D Regueiro, MD1. P4369 - GLP-1 Agonists are Associated With Lower Rates of IBD-Related Complications in Patients With Elevated BMI Compared to Bariatric Surgery: A Nationwide Cohort Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2University of Aleppo, Cleveland, OH; 3Chicago Medical School at Rosalind Franklin University of Medicine and Science, Chicago, IL; 4Landmark Medical Center, Cumberland, RI
Introduction: The prevalence of obesity is rising worldwide with a parallel rise in inflammatory bowel disease (IBD). Studies on the impact of obesity on IBD are conflicting, but some suggest increased adverse events in IBD population with obesity with suggested improved outcomes in obese IBD patients undergoing bariatric surgery. Glucagon-like peptide (GLP-1) agonists are rapidly emerging as a less invasive alternative to bariatric surgery for the management of obesity with recent studies showing improved IBD outcomes with the use of GLP-1 agonists. However, GLP-1 agonists were never directly compared to bariatric surgery in obese IBD patients.
Methods: This is a retrospective cohort analysis using TrinetX, a database pulling from 80 healthcare organizations across the United States. Adult patients with IBD were identified using ICD-10 codes. Cohort was divided into patients with GLP-1 agonists prescription (dulaglutide, semaglutide, liraglutide, lixisenatide, exenatide or tirzepatide) who never underwent bariatric surgery and patients who underwent bariatric surgery but never received GLP-1 agonists. Cohorts were propensity score matched using demographics, comorbidities and IBD medications.
Results: A total of 189,703 obese IBD patient were found. Of which, around 15,000 patients got GLP-1 vs 1,240 underwent bariatric surgery. GLP-1 group were older at index (55 vs 47) year-old respectively. GLP-1 patients had higher rates of co-morbidities including diabetes (60% vs 28%), chronic kidney disease (14% vs 6%), cerebrovascular accident (10% vs 5%) and ischemic heart disease (22% vs 12%) but lower mood disorder (40% vs 50%) and anxiety rates (38% vs 40%) respectively compared to the bariatric group. GLP-1 agonists group also had higher rates of IBD related medications including steroids (71% vs 56%) and mesalamine (20% vs 14%) respectively. After propensity score matching, GLP-1 patients had significantly lower odds of emergency visits/hospitalization (OR 0.5), fistulas (OR 0.26), intestinal obstruction (OR 0.32), deep venous thrombosis (OR 0.54), pulmonary embolism (0.45), C-diff infection (0.5) and mortality (OR 0.31) but higher need for biologics (OR 1.42) despite having higher BMI mean compared to bariatric surgery group (36.4 vs 33.6).
Discussion: Obese IBD patients on GLP-1 agonists had higher rates of comorbidities but less IBD related complications compared to patients who received bariatric surgery despite higher mean BMI.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
M Housam Nanah indicated no relevant financial relationships.
Robana Nanah indicated no relevant financial relationships.
Rama Nanah indicated no relevant financial relationships.
Rashid Abdel-Razeq indicated no relevant financial relationships.
Gauri Pikale indicated no relevant financial relationships.
Abdullah Hafeez indicated no relevant financial relationships.
Miguel D Regueiro: AbbVie – Advisory Committee/Board Member, Consultant, Speakers Bureau.
M Housam Nanah, MD1, Robana Nanah, MD2, Rama Nanah, MD1, Rashid Abdel-Razeq, MD1, Gauri Pikale, MD3, Abdullah Hafeez, MD4, Miguel D Regueiro, MD1. P4369 - GLP-1 Agonists are Associated With Lower Rates of IBD-Related Complications in Patients With Elevated BMI Compared to Bariatric Surgery: A Nationwide Cohort Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

