Tuesday Poster Session
Category: IBD
P4376 - H pylori: A Bane or Boon? Impact of H. pylori Infection on Outcomes in Inflammatory Bowel Disease
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Charmy Parikh, MD
Mercy Catholic Medical Center
Darby, PA
Presenting Author(s)
Raj H. Patel, MD1, Charmy Parikh, MD2, Sneh Sonaiya, MD3, Pratiksha Moliya, MD4, Yash R. Shah, MD5, Umang Patel, MD6
1St. Mary Medical Center, Bensalem, PA; 2Mercy Catholic Medical Center, Darby, PA; 3University of Nevada, Las Vegas, NV; 4Jamaica Hospital Medical Center, Queens, NY; 5Trinity Health Oakland / Wayne State University School of Medicine, Pontiac, MI; 6St. Mary Medical Center, Langhorne, PA
Introduction: H. pylori colonizes more than fifty percent of the world's population, and is usually considered commensal, it has been associated with illnesses such as gastritis, ulcers, and cancer of the gastric carcinoma. Prior studies indicate that infection with H. pylori may provide a safeguarding effect against autoimmune disorders by enhancing immunological tolerance and reducing inflammatory reactions. Our retrospective study is intended to investigate the influence of H. pylori infection on outcomes in hospitalized patients with inflammatory bowel disease (IBD).
Methods: A retrospective analysis was carried out using the National Inpatient Sample (NIS) database from 2016 to
2020 to examine the influence of H. pylori infection on outcomes in hospitalized patients with
inflammatory bowel disease (IBD). The study primarily investigated the impact of H. pylori infection on
death rates, duration of hospital admissions, and related expenses. In this study, we additionally examined
a range of predictive outcomes to thoroughly evaluate the wider consequences of H. pylori prevalence in
patients with inflammatory bowel disease (IBD).
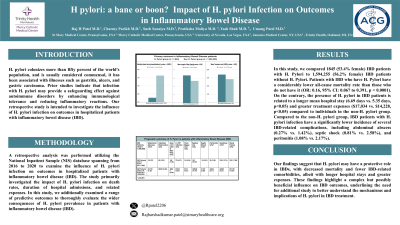
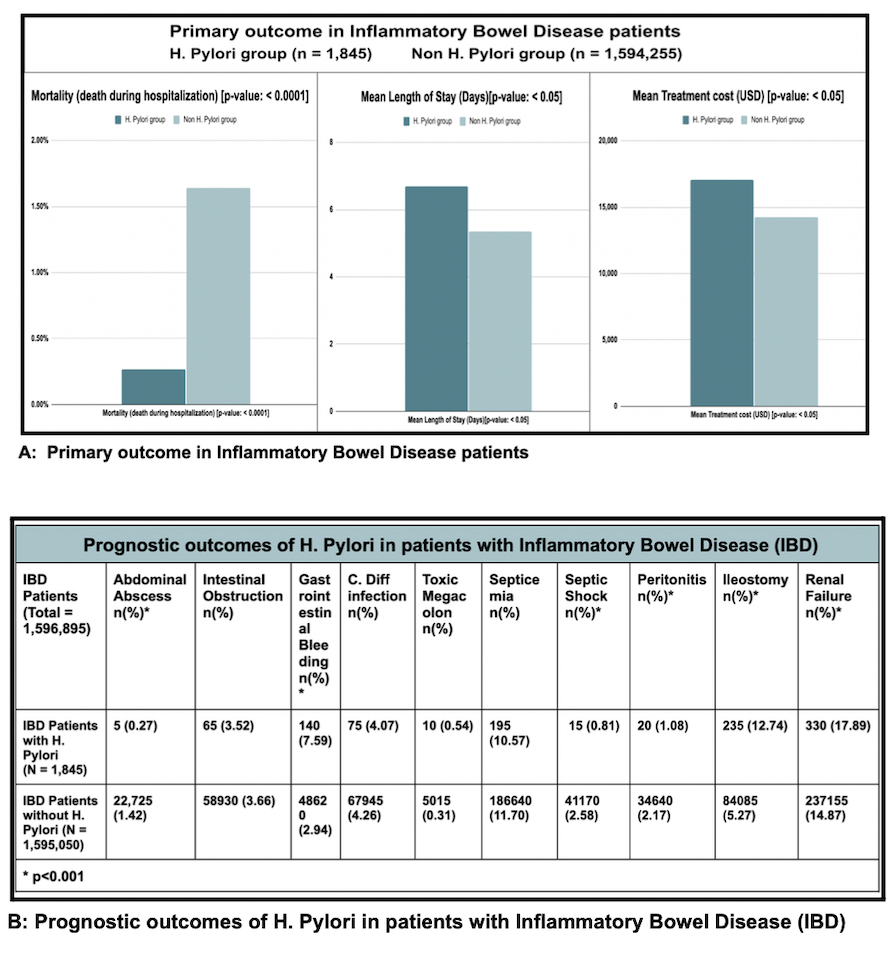
Results: In this study, we compared 1845 (53.4% female) IBD patients with H. Pylori to 1,594,255 (56.2% female)
IBD patients without H. Pylori. Patients with IBD who have H. Pylori have a considerably lower all-cause
mortality rate than those who do not have it (OR: 0.16, 95% CI: 0.067 to 0.391, p < 0.0001). On the
contrary, the presence of H. pylori in IBD patients is related to a longer mean hospital stay (6.69 days vs.
5.35 days, p< 0.05) and greater treatment expenses ($17,034 vs. $14,228, p< 0.05) compared to individuals
in the non-H. pylori group. Compared to the non-H. pylori group, IBD patients with H. pylori infection
have a significantly lower incidence of several IBD-related complications, including abdominal abscess
(0.27% vs. 1.42%), septic shock (0.81% vs. 2.58%), and peritonitis (1.08% vs. 2.17%).
Discussion: Our findings suggest that H. pylori may have a protective role in IBDs, with decreased mortality
and fewer IBD-related comorbidities, albeit with longer hospital stays and greater expenses.
These findings highlight a complex but possibly beneficial influence on IBD outcomes,
underlining the need for additional study to better understand the mechanisms and implications
of H. pylori in IBD treatment.
Disclosures:
Raj H. Patel, MD1, Charmy Parikh, MD2, Sneh Sonaiya, MD3, Pratiksha Moliya, MD4, Yash R. Shah, MD5, Umang Patel, MD6. P4376 - H pylori: A Bane or Boon? Impact of H. pylori Infection on Outcomes in Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1St. Mary Medical Center, Bensalem, PA; 2Mercy Catholic Medical Center, Darby, PA; 3University of Nevada, Las Vegas, NV; 4Jamaica Hospital Medical Center, Queens, NY; 5Trinity Health Oakland / Wayne State University School of Medicine, Pontiac, MI; 6St. Mary Medical Center, Langhorne, PA
Introduction: H. pylori colonizes more than fifty percent of the world's population, and is usually considered commensal, it has been associated with illnesses such as gastritis, ulcers, and cancer of the gastric carcinoma. Prior studies indicate that infection with H. pylori may provide a safeguarding effect against autoimmune disorders by enhancing immunological tolerance and reducing inflammatory reactions. Our retrospective study is intended to investigate the influence of H. pylori infection on outcomes in hospitalized patients with inflammatory bowel disease (IBD).
Methods: A retrospective analysis was carried out using the National Inpatient Sample (NIS) database from 2016 to
2020 to examine the influence of H. pylori infection on outcomes in hospitalized patients with
inflammatory bowel disease (IBD). The study primarily investigated the impact of H. pylori infection on
death rates, duration of hospital admissions, and related expenses. In this study, we additionally examined
a range of predictive outcomes to thoroughly evaluate the wider consequences of H. pylori prevalence in
patients with inflammatory bowel disease (IBD).
Results: In this study, we compared 1845 (53.4% female) IBD patients with H. Pylori to 1,594,255 (56.2% female)
IBD patients without H. Pylori. Patients with IBD who have H. Pylori have a considerably lower all-cause
mortality rate than those who do not have it (OR: 0.16, 95% CI: 0.067 to 0.391, p < 0.0001). On the
contrary, the presence of H. pylori in IBD patients is related to a longer mean hospital stay (6.69 days vs.
5.35 days, p< 0.05) and greater treatment expenses ($17,034 vs. $14,228, p< 0.05) compared to individuals
in the non-H. pylori group. Compared to the non-H. pylori group, IBD patients with H. pylori infection
have a significantly lower incidence of several IBD-related complications, including abdominal abscess
(0.27% vs. 1.42%), septic shock (0.81% vs. 2.58%), and peritonitis (1.08% vs. 2.17%).
Discussion: Our findings suggest that H. pylori may have a protective role in IBDs, with decreased mortality
and fewer IBD-related comorbidities, albeit with longer hospital stays and greater expenses.
These findings highlight a complex but possibly beneficial influence on IBD outcomes,
underlining the need for additional study to better understand the mechanisms and implications
of H. pylori in IBD treatment.
Figure: Outcomes in Hospitalized IBD Patients with and without H. Pylori Infection
Disclosures:
Raj Patel indicated no relevant financial relationships.
Charmy Parikh indicated no relevant financial relationships.
Sneh Sonaiya indicated no relevant financial relationships.
Pratiksha Moliya indicated no relevant financial relationships.
Yash Shah indicated no relevant financial relationships.
Umang Patel indicated no relevant financial relationships.
Raj H. Patel, MD1, Charmy Parikh, MD2, Sneh Sonaiya, MD3, Pratiksha Moliya, MD4, Yash R. Shah, MD5, Umang Patel, MD6. P4376 - H pylori: A Bane or Boon? Impact of H. pylori Infection on Outcomes in Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
