Tuesday Poster Session
Category: IBD
P4384 - Comparative Impact of COVID-19 on Patients With vs Without Inflammatory Bowel Disease in the United States
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SZ
Sheng Zhou, MD, MS
University at Buffalo
Depew, NY
Presenting Author(s)
Sheng Zhou, MD, MS1, Shaniza Haniff, MD, MPH1, Netanel Krugliak, 2, Samir Shah, MD3
1University at Buffalo, Buffalo, NY; 2Xavier University School of Medicine, Toronto, ON, Canada; 3Gastroenterology Associates, Providence, RI
Introduction: Prior research has presented conflicting findings on whether COVID-19 impacts individuals with Inflammatory Bowel Disease (IBD) differently than the general population. Notably, comprehensive nationwide studies are lacking in the United States. This study seeks to bridge this gap by quantifying and comparing the effects of COVID-19 between the IBD and non-IBD populations.
Methods: A retrospective cohort study was conducted using the 2020 Nationwide Readmissions Database from the Healthcare Cost and Utilization Project (HCUP). The study included all adult patients hospitalized from January 1, 2020, to December 31, 2020. Outcomes assessed were inpatient mortality, 30-day readmission, and length of stay (LoS). Logistic regressions were used to calculate odds ratios (OR) for binary outcomes. Negative binomial regression was used to calculate the incidence rate ratio (IRR) for LoS. Adjustments were made for age, gender, anemia, heart disease, hypertension, lung disease, coronary vascular disease, gastrointestinal bleeding, endocrine disorders, drug abuse, other infections, kidney disease, and hypoalbuminemia using ICD-10 codes and the HCUP Clinical Classifications Software Refined tool.
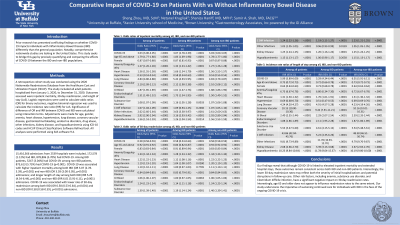
Results: The study analyzed 15,416,366 admissions from 2,539 hospitals, 172,578 (1.12%) admissions with IBD patients, and 878,806 (5.70%) admissions had COVID-19. Among IBD patients, 5247 (3.04%) had COVID-19 compared to 873,613 (5.73%) among non-IBD patients (p< 0.001). COVID-19 was associated with higher inpatient mortality among both IBD (OR 3.07, 95% CI 2.78-3.39, p< 0.001) and non-IBD (OR 3.03, 95% CI 3.00-3.05, p< 0.001) admissions (Table 1). Additionally, COVID-19 led to longer LoS in both groups (IBD: IRR 5.29, 95% CI 4.34-6.44, p< 0.001; non-IBD: IRR 6.01, 95% CI 5.91-6.11, p< 0.001). However, COVID-19 was linked to a lower rate of 30-day readmission in both IBD (OR 0.58, 95% CI 0.53-0.64, p< 0.001) and non-IBD (OR 0.58, 95% CI 0.58-0.59, p< 0.001) populations.
Discussion: Our findings reveal that although COVID-19 is linked to elevated inpatient mortality and extended hospital stays, these outcomes remain consistent across both IBD and non-IBD patients. This is consistent with other studies and should be reassuring to patients with IBD. The observed reduction in 30-day readmission rates may suggest recovery and subsequent immunity from COVID-19, although further research is needed in this area.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sheng Zhou, MD, MS1, Shaniza Haniff, MD, MPH1, Netanel Krugliak, 2, Samir Shah, MD3. P4384 - Comparative Impact of COVID-19 on Patients With vs Without Inflammatory Bowel Disease in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University at Buffalo, Buffalo, NY; 2Xavier University School of Medicine, Toronto, ON, Canada; 3Gastroenterology Associates, Providence, RI
Introduction: Prior research has presented conflicting findings on whether COVID-19 impacts individuals with Inflammatory Bowel Disease (IBD) differently than the general population. Notably, comprehensive nationwide studies are lacking in the United States. This study seeks to bridge this gap by quantifying and comparing the effects of COVID-19 between the IBD and non-IBD populations.
Methods: A retrospective cohort study was conducted using the 2020 Nationwide Readmissions Database from the Healthcare Cost and Utilization Project (HCUP). The study included all adult patients hospitalized from January 1, 2020, to December 31, 2020. Outcomes assessed were inpatient mortality, 30-day readmission, and length of stay (LoS). Logistic regressions were used to calculate odds ratios (OR) for binary outcomes. Negative binomial regression was used to calculate the incidence rate ratio (IRR) for LoS. Adjustments were made for age, gender, anemia, heart disease, hypertension, lung disease, coronary vascular disease, gastrointestinal bleeding, endocrine disorders, drug abuse, other infections, kidney disease, and hypoalbuminemia using ICD-10 codes and the HCUP Clinical Classifications Software Refined tool.
Results: The study analyzed 15,416,366 admissions from 2,539 hospitals, 172,578 (1.12%) admissions with IBD patients, and 878,806 (5.70%) admissions had COVID-19. Among IBD patients, 5247 (3.04%) had COVID-19 compared to 873,613 (5.73%) among non-IBD patients (p< 0.001). COVID-19 was associated with higher inpatient mortality among both IBD (OR 3.07, 95% CI 2.78-3.39, p< 0.001) and non-IBD (OR 3.03, 95% CI 3.00-3.05, p< 0.001) admissions (Table 1). Additionally, COVID-19 led to longer LoS in both groups (IBD: IRR 5.29, 95% CI 4.34-6.44, p< 0.001; non-IBD: IRR 6.01, 95% CI 5.91-6.11, p< 0.001). However, COVID-19 was linked to a lower rate of 30-day readmission in both IBD (OR 0.58, 95% CI 0.53-0.64, p< 0.001) and non-IBD (OR 0.58, 95% CI 0.58-0.59, p< 0.001) populations.
Discussion: Our findings reveal that although COVID-19 is linked to elevated inpatient mortality and extended hospital stays, these outcomes remain consistent across both IBD and non-IBD patients. This is consistent with other studies and should be reassuring to patients with IBD. The observed reduction in 30-day readmission rates may suggest recovery and subsequent immunity from COVID-19, although further research is needed in this area.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sheng Zhou indicated no relevant financial relationships.
Shaniza Haniff indicated no relevant financial relationships.
Netanel Krugliak indicated no relevant financial relationships.
Samir Shah: Roche Information Systems – Consultant.
Sheng Zhou, MD, MS1, Shaniza Haniff, MD, MPH1, Netanel Krugliak, 2, Samir Shah, MD3. P4384 - Comparative Impact of COVID-19 on Patients With vs Without Inflammatory Bowel Disease in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

