Tuesday Poster Session
Category: IBD
P4385 - A Reevaluation of Clostridioides difficile Impact on Hospitalized IBD Patients in the United States: Disproving the Notion of Worst Outcome
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SZ
Sheng Zhou, MD, MS
University at Buffalo
Depew, NY
Presenting Author(s)
Sheng Zhou, MD, MS1, Manasik Abdu, MD2, Netanel Krugliak, 3, Samir A. Shah, MD4
1University at Buffalo, Buffalo, NY; 2UB Jacobs School of Medicine, Buffalo, NY; 3Xavier University School of Medicine, Toronto, ON, Canada; 4Gastroenterology Associates, Inc., powered by GI Alliance, Providence, RI
Introduction: Clostridium difficile (C. Diff) infection in inflammatory bowel disease (IBD) patients has been recognized for its increased prevalence and worse outcomes. Recent data examining these associations are lacking. We aim to fill this gap by investigating the impact of C. Diff on various outcomes among IBD.
Methods: This retrospective cohort study included all adult IBD patients hospitalized between 1/1/2020-12/31/2020 across the United States. Outcomes including inpatient death, 30-day readmission, length of stay (LoS), discharge to home, colonoscopy, toxic megacolon, perforation, and colectomy during hospitalization were compared among those with C. Diff vs. those without. Odds ratios were calculated using logistic regressions for binary outcomes. Incidence rate ratio was calculated using negative binomial regression for LoS. These were adjusted for risk factors listed in the table. Outcomes and risk factors were identified using ICD 10 codes. The data source is the 2020 Nationwide Readmissions Database from HCUP.
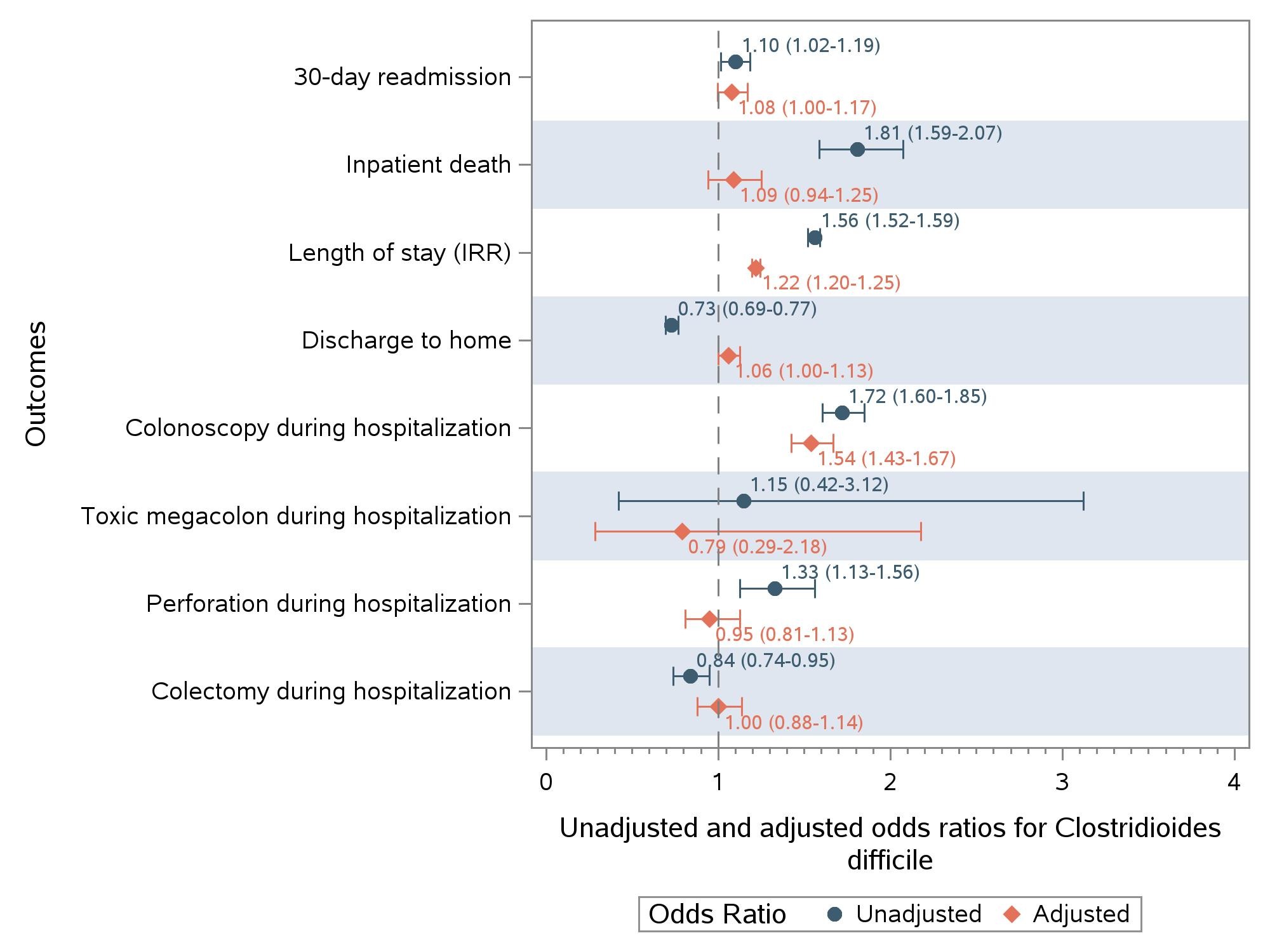
Results: A total of 172,578 admissions from 2,319 hospitals were included comprising 60.7% Crohn’s disease, 37.6% ulcerative colitis, and 2.6% other IBD. C. Diff infection was more prevalent among those with IBD compared to those without (3.54% vs. 0.73%, p< 0.001). Demographics and comorbidities were compared between those with and without C. Diff (table). Before adjustment, C. Diff was associated with higher mortality, readmission rates, LoS, increased likelihood of bowel perforation, and decreased likelihood of colectomy during hospitalization. After adjusting for risk factors in the table, IBD patients with C. Diff had 22% longer LoS, and were 54% more likely to get colonoscopy during hospitalization compared to those without. There was no difference for other outcomes.
Discussion: Our findings revealed that C. Diff infection does not correlate with elevated rates of inpatient mortality, perforation, toxic megacolon, colectomy, or readmission among IBD patients. However, it is associated with extended LoS. With advancements in treatment options, C. Diff does not appear be associated with higher rates of colectomy or death. However, it still poses a higher healthcare burden with longer length of stay. Our study is limited by its retrospective nature and reliance on database and coding. These results underscore the ongoing imperative to focus efforts to prevent the acquisition of C. Diff among IBD patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sheng Zhou, MD, MS1, Manasik Abdu, MD2, Netanel Krugliak, 3, Samir A. Shah, MD4. P4385 - A Reevaluation of <i>Clostridioides difficile</i> Impact on Hospitalized IBD Patients in the United States: Disproving the Notion of Worst Outcome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University at Buffalo, Buffalo, NY; 2UB Jacobs School of Medicine, Buffalo, NY; 3Xavier University School of Medicine, Toronto, ON, Canada; 4Gastroenterology Associates, Inc., powered by GI Alliance, Providence, RI
Introduction: Clostridium difficile (C. Diff) infection in inflammatory bowel disease (IBD) patients has been recognized for its increased prevalence and worse outcomes. Recent data examining these associations are lacking. We aim to fill this gap by investigating the impact of C. Diff on various outcomes among IBD.
Methods: This retrospective cohort study included all adult IBD patients hospitalized between 1/1/2020-12/31/2020 across the United States. Outcomes including inpatient death, 30-day readmission, length of stay (LoS), discharge to home, colonoscopy, toxic megacolon, perforation, and colectomy during hospitalization were compared among those with C. Diff vs. those without. Odds ratios were calculated using logistic regressions for binary outcomes. Incidence rate ratio was calculated using negative binomial regression for LoS. These were adjusted for risk factors listed in the table. Outcomes and risk factors were identified using ICD 10 codes. The data source is the 2020 Nationwide Readmissions Database from HCUP.
Results: A total of 172,578 admissions from 2,319 hospitals were included comprising 60.7% Crohn’s disease, 37.6% ulcerative colitis, and 2.6% other IBD. C. Diff infection was more prevalent among those with IBD compared to those without (3.54% vs. 0.73%, p< 0.001). Demographics and comorbidities were compared between those with and without C. Diff (table). Before adjustment, C. Diff was associated with higher mortality, readmission rates, LoS, increased likelihood of bowel perforation, and decreased likelihood of colectomy during hospitalization. After adjusting for risk factors in the table, IBD patients with C. Diff had 22% longer LoS, and were 54% more likely to get colonoscopy during hospitalization compared to those without. There was no difference for other outcomes.
Discussion: Our findings revealed that C. Diff infection does not correlate with elevated rates of inpatient mortality, perforation, toxic megacolon, colectomy, or readmission among IBD patients. However, it is associated with extended LoS. With advancements in treatment options, C. Diff does not appear be associated with higher rates of colectomy or death. However, it still poses a higher healthcare burden with longer length of stay. Our study is limited by its retrospective nature and reliance on database and coding. These results underscore the ongoing imperative to focus efforts to prevent the acquisition of C. Diff among IBD patients.
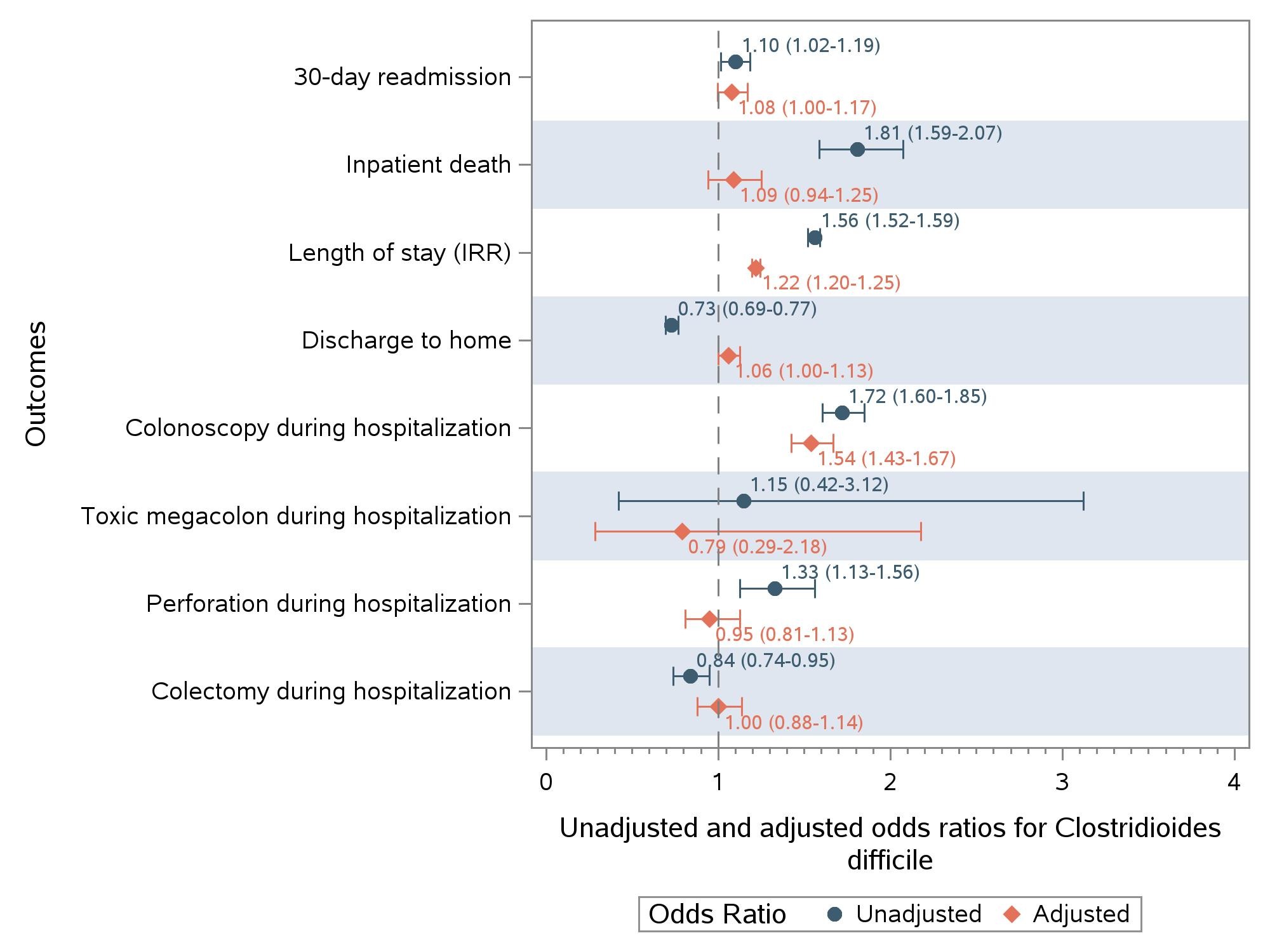
Figure: Associations between Clotridoides difficile and Outcomes
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sheng Zhou indicated no relevant financial relationships.
Manasik Abdu indicated no relevant financial relationships.
Netanel Krugliak indicated no relevant financial relationships.
Samir Shah: Roche Information Systems – Consultant.
Sheng Zhou, MD, MS1, Manasik Abdu, MD2, Netanel Krugliak, 3, Samir A. Shah, MD4. P4385 - A Reevaluation of <i>Clostridioides difficile</i> Impact on Hospitalized IBD Patients in the United States: Disproving the Notion of Worst Outcome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

