Tuesday Poster Session
Category: IBD
P4387 - Investigating the Natural Progression of Microscopic Colitis: Analysis of the Loyola University Microscopic Colitis Registry (LUMiCoR)
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Karolina Krawczyk, MD, MS
Loyola University Medical Center
Harwood Heights, IL
Presenting Author(s)
Karolina Krawczyk, MD, MS1, Christopher Kujalowicz, BS2, Dinkar Ahuja, MD3, Mohammed Abourahma, MD3, Ayokunle T. Abegunde, MD, MSc, MRCP, FACG3
1Loyola University Medical Center, Harwood Heights, IL; 2Loyola University Chicago Stritch School of Medicine, Maywood, IL; 3Loyola University Medical Center, Maywood, IL
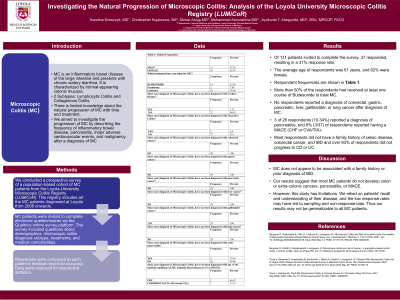
Introduction: Microscopic colitis (MC) is an inflammatory bowel disease (IBD) of the large intestine that presents as chronic watery diarrhea; it is characterized by normal-appearing colonic mucosa and it has two histologic subtypes: lymphocytic colitis (LC) and collagenous colitis (CC). There is limited knowledge about the natural progression of MC with time and with treatment. We aimed to investigate the progression of MC by describing the frequency of inflammatory bowel disease, pancreatitis, major adverse cardiovascular events, and malignancy after a diagnosis of MC.
Methods: We conducted a prospective survey of a population-based cohort of MC patients from the Loyola University Microscopic Colitis Registry (LUMiCoR). The registry includes all MC patients diagnosed at Loyola from 2008 and onwards. MC patients were invited to complete electronic questionnaires via the Qualtrics online survey platform. The survey included questions about demographics, microscopic colitis diagnosis subtype, treatments, and medical comorbidities. Responses were compared to each patient’s medical record for accuracy. Data were analyzed for descriptive statistics.
Results: Of 121 patients invited to complete the survey, 37 responded, resulting in a 31% response rate. The average age of respondents was 61 years, and 62% were female. Respondent frequencies are shown in Table 1. More than 50% of the respondents had received at least one course of Budesonide to treat MC. No respondents reported a diagnosis of colorectal, gastric, pancreatic, liver, gallbladder, or lung cancer after diagnosis of MC. Three of twenty-six respondents (10.34%) reported a diagnosis of pancreatitis, and 8% (3/37) of respondents reported having a MACE (CHF or CVA/TIA). The majority of respondents did not have a family history of celiac disease, colorectal cancer, and IBD and over 93% of respondents did not progress to CD or UC.
Discussion: MC does not appear to be associated with a family history or prior diagnosis of IBD. Our results suggest that the majority of MC patients do not develop colon or extra-colonic cancers, pancreatitis, or MACE. However, this study has limitations. We relied on patients' recall and understanding of their disease, and the low response rates may have led to sampling and non-response bias in our data.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Karolina Krawczyk, MD, MS1, Christopher Kujalowicz, BS2, Dinkar Ahuja, MD3, Mohammed Abourahma, MD3, Ayokunle T. Abegunde, MD, MSc, MRCP, FACG3. P4387 - Investigating the Natural Progression of Microscopic Colitis: Analysis of the Loyola University Microscopic Colitis Registry (LUMiCoR), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Loyola University Medical Center, Harwood Heights, IL; 2Loyola University Chicago Stritch School of Medicine, Maywood, IL; 3Loyola University Medical Center, Maywood, IL
Introduction: Microscopic colitis (MC) is an inflammatory bowel disease (IBD) of the large intestine that presents as chronic watery diarrhea; it is characterized by normal-appearing colonic mucosa and it has two histologic subtypes: lymphocytic colitis (LC) and collagenous colitis (CC). There is limited knowledge about the natural progression of MC with time and with treatment. We aimed to investigate the progression of MC by describing the frequency of inflammatory bowel disease, pancreatitis, major adverse cardiovascular events, and malignancy after a diagnosis of MC.
Methods: We conducted a prospective survey of a population-based cohort of MC patients from the Loyola University Microscopic Colitis Registry (LUMiCoR). The registry includes all MC patients diagnosed at Loyola from 2008 and onwards. MC patients were invited to complete electronic questionnaires via the Qualtrics online survey platform. The survey included questions about demographics, microscopic colitis diagnosis subtype, treatments, and medical comorbidities. Responses were compared to each patient’s medical record for accuracy. Data were analyzed for descriptive statistics.
Results: Of 121 patients invited to complete the survey, 37 responded, resulting in a 31% response rate. The average age of respondents was 61 years, and 62% were female. Respondent frequencies are shown in Table 1. More than 50% of the respondents had received at least one course of Budesonide to treat MC. No respondents reported a diagnosis of colorectal, gastric, pancreatic, liver, gallbladder, or lung cancer after diagnosis of MC. Three of twenty-six respondents (10.34%) reported a diagnosis of pancreatitis, and 8% (3/37) of respondents reported having a MACE (CHF or CVA/TIA). The majority of respondents did not have a family history of celiac disease, colorectal cancer, and IBD and over 93% of respondents did not progress to CD or UC.
Discussion: MC does not appear to be associated with a family history or prior diagnosis of IBD. Our results suggest that the majority of MC patients do not develop colon or extra-colonic cancers, pancreatitis, or MACE. However, this study has limitations. We relied on patients' recall and understanding of their disease, and the low response rates may have led to sampling and non-response bias in our data.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Karolina Krawczyk indicated no relevant financial relationships.
Christopher Kujalowicz indicated no relevant financial relationships.
Dinkar Ahuja indicated no relevant financial relationships.
Mohammed Abourahma indicated no relevant financial relationships.
Ayokunle Abegunde: Ferring Pharmaceuticals – Consultant. Ferring Pharmaceuticals – Consultant.
Karolina Krawczyk, MD, MS1, Christopher Kujalowicz, BS2, Dinkar Ahuja, MD3, Mohammed Abourahma, MD3, Ayokunle T. Abegunde, MD, MSc, MRCP, FACG3. P4387 - Investigating the Natural Progression of Microscopic Colitis: Analysis of the Loyola University Microscopic Colitis Registry (LUMiCoR), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
