Tuesday Poster Session
Category: IBD
P4403 - Prevalence and Outcomes of Active and Latent Tuberculosis Among Patients With Inflammatory Bowel Disease (IBD) in an Endemic Region
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Badr Al Bawardy, MD
King Faisal Specialist Hospital and Research Centre
Riyadh, Ar Riyad, Saudi Arabia
Presenting Author(s)
Mohammed Alayed, MBBS, Abdulrahman Alrasheed, MBBS, Muath Alenezi, MBBS, Ibrahim Binsalmah, , Abdulelah Almutairdi, MD, Mashary Attamimi, MD, Badr Al-Bawardy, MD
King Faisal Specialist Hospital and Research Centre, Riyadh, Ar Riyad, Saudi Arabia
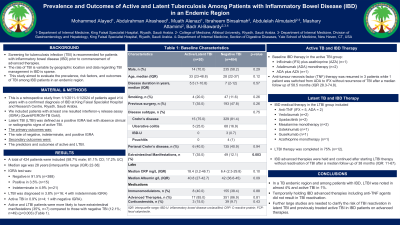
Introduction: Screening for tuberculosis infection (TBI) is recommended for patients with inflammatory bowel disease (IBD) prior to commencement of advanced therapies. The rate of TBI is variable by geographic location and data regarding TBI management in IBD is sparse. We aimed to evaluate the prevalence, risk factors and outcomes of TBI among IBD patients in an endemic region.
Methods: This is a retrospective study from 1/1/2011-1/1/2024 of patients aged ≥14 years with a confirmed diagnosis of IBD at King Faisal Specialist Hospital and Research Centre, Riyadh, Saudi Arabia. We included patients with at least on resulted interferon-γ release assay (IGRA) (QuantiFERON-TB Gold). Latent TBI (LTBI) was defined as a positive IGRA test with absence clinical or radiographic signs of active TBI. The primary outcome was the rate of negative, indeterminate, and positive IGRA. Secondary outcomes included predictors and outcomes of active and LTBI.
Results: A total of 424 patients with IBD (58.7% male; 81.1% Crohn’s disease; 17.2% ulcerative colitis) with a median age of 28 years [interquartile range (IQR) 22-38] were included. IGRA test was negative in 91.5% (n=388), positive in 3.5% (n=15) and indeterminate in 4.9% (n=21). LTBI was diagnosed in 3.8% (n=16; 4 with indeterminate IGRA) and active TBI in 0.9% (n=4; 1 with negative IGRA). Active and LTBI patients were more likely to have extraintestinal manifestations (35%, n=7) compared to those with negative TBI (12.1%; n=49) (p=0.003) (Table 1).
Baseline IBD therapy in the active TBI included infliximab (IFX) plus azathioprine (AZA) (n=1), adalimumab (ADA) monotherapy (n=2) and ADA plus AZA (n=1). Anti-tumour necrosis factor (TNF) therapy was resumed in 3 patients while 1 patient was switched from ADA to IFX without recurrence of TBI after a median follow up of 58.5 months (IQR 28.3-74.8).
In the LTBI group, 43.8% were on anti-TNF (IFX = 5, ADA = 2), 12.5% on vedolizumab, 6.3% on ustekinumab, 6.3% on guselkumab, and 12.5% on upadacitinib. Two patients were treated with mesalamine monotherapy and one with AZA. LTBI therapy was completed in 75% (n=12). IBD advanced therapies were held and continued after starting LTBI therapy without reactivation of TBI after a median follow up of 38 months (IQR: 11-67).
Discussion: In a TB endemic region and among patients with IBD, LTBI was noted in almost 4% and active TBI in 1%. Temporarily holding IBD advanced therapies including anti-TNF agents did not result in TBI reactivation.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mohammed Alayed, MBBS, Abdulrahman Alrasheed, MBBS, Muath Alenezi, MBBS, Ibrahim Binsalmah, , Abdulelah Almutairdi, MD, Mashary Attamimi, MD, Badr Al-Bawardy, MD. P4403 - Prevalence and Outcomes of Active and Latent Tuberculosis Among Patients With Inflammatory Bowel Disease (IBD) in an Endemic Region, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
King Faisal Specialist Hospital and Research Centre, Riyadh, Ar Riyad, Saudi Arabia
Introduction: Screening for tuberculosis infection (TBI) is recommended for patients with inflammatory bowel disease (IBD) prior to commencement of advanced therapies. The rate of TBI is variable by geographic location and data regarding TBI management in IBD is sparse. We aimed to evaluate the prevalence, risk factors and outcomes of TBI among IBD patients in an endemic region.
Methods: This is a retrospective study from 1/1/2011-1/1/2024 of patients aged ≥14 years with a confirmed diagnosis of IBD at King Faisal Specialist Hospital and Research Centre, Riyadh, Saudi Arabia. We included patients with at least on resulted interferon-γ release assay (IGRA) (QuantiFERON-TB Gold). Latent TBI (LTBI) was defined as a positive IGRA test with absence clinical or radiographic signs of active TBI. The primary outcome was the rate of negative, indeterminate, and positive IGRA. Secondary outcomes included predictors and outcomes of active and LTBI.
Results: A total of 424 patients with IBD (58.7% male; 81.1% Crohn’s disease; 17.2% ulcerative colitis) with a median age of 28 years [interquartile range (IQR) 22-38] were included. IGRA test was negative in 91.5% (n=388), positive in 3.5% (n=15) and indeterminate in 4.9% (n=21). LTBI was diagnosed in 3.8% (n=16; 4 with indeterminate IGRA) and active TBI in 0.9% (n=4; 1 with negative IGRA). Active and LTBI patients were more likely to have extraintestinal manifestations (35%, n=7) compared to those with negative TBI (12.1%; n=49) (p=0.003) (Table 1).
Baseline IBD therapy in the active TBI included infliximab (IFX) plus azathioprine (AZA) (n=1), adalimumab (ADA) monotherapy (n=2) and ADA plus AZA (n=1). Anti-tumour necrosis factor (TNF) therapy was resumed in 3 patients while 1 patient was switched from ADA to IFX without recurrence of TBI after a median follow up of 58.5 months (IQR 28.3-74.8).
In the LTBI group, 43.8% were on anti-TNF (IFX = 5, ADA = 2), 12.5% on vedolizumab, 6.3% on ustekinumab, 6.3% on guselkumab, and 12.5% on upadacitinib. Two patients were treated with mesalamine monotherapy and one with AZA. LTBI therapy was completed in 75% (n=12). IBD advanced therapies were held and continued after starting LTBI therapy without reactivation of TBI after a median follow up of 38 months (IQR: 11-67).
Discussion: In a TB endemic region and among patients with IBD, LTBI was noted in almost 4% and active TBI in 1%. Temporarily holding IBD advanced therapies including anti-TNF agents did not result in TBI reactivation.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mohammed Alayed indicated no relevant financial relationships.
Abdulrahman Alrasheed indicated no relevant financial relationships.
Muath Alenezi indicated no relevant financial relationships.
Ibrahim Binsalmah indicated no relevant financial relationships.
Abdulelah Almutairdi indicated no relevant financial relationships.
Mashary Attamimi indicated no relevant financial relationships.
Badr Al-Bawardy: AbbVie – Consultant, Speakers Bureau. Janssen – Speakers Bureau. Pfizer – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Takeda – Speakers Bureau.
Mohammed Alayed, MBBS, Abdulrahman Alrasheed, MBBS, Muath Alenezi, MBBS, Ibrahim Binsalmah, , Abdulelah Almutairdi, MD, Mashary Attamimi, MD, Badr Al-Bawardy, MD. P4403 - Prevalence and Outcomes of Active and Latent Tuberculosis Among Patients With Inflammatory Bowel Disease (IBD) in an Endemic Region, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
