Tuesday Poster Session
Category: IBD
P4405 - Cerebral Venous Thrombosis as an Initial Presentation of Ulcerative Colitis: A Case Report and Literature Review
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AB
Abakar Baraka, MD
University of Colorado-Anschutz Campus
San Antonio, TX
Presenting Author(s)
Abakar Baraka, MD1, Benjamin Heriford, DO2, Jawairia Memon, MD3, Diego Cebrian, MD4
1University of Colorado-Anschutz Campus, San Antonio, TX; 2UTHSCSA, San Antonio, TX; 3University of Texas Health Science Center, San Antonio, TX; 4University of Texas Health San Antonio, San Antonio, TX
Introduction: Cerebral venous thrombosis (CVT) is a rare but significant neurological condition often leading to severe complications such as stroke. While CVT can result from various etiologies, its association with systemic inflammatory diseases like inflammatory bowel disease (IBD), particularly ulcerative colitis (UC), has garnered increasing clinical attention. This case report explores CVT as an initial extraintestinal manifestation of UC, highlighting the diagnostic challenges and the need for considering IBD in the differential diagnosis of CVT.
Case Description/Methods: A 26-year-old female with no significant past medical history, aside from oral contraceptive pill use, presented with recent gastrointestinal symptoms characterized by diarrhea with intermittent hematochezia and melena. Her symptoms progressed over several weeks, eventually leading to severe headaches, right-sided weakness, and dysarthria. Acute neurological decline manifested as seizures, prompting urgent medical attention.
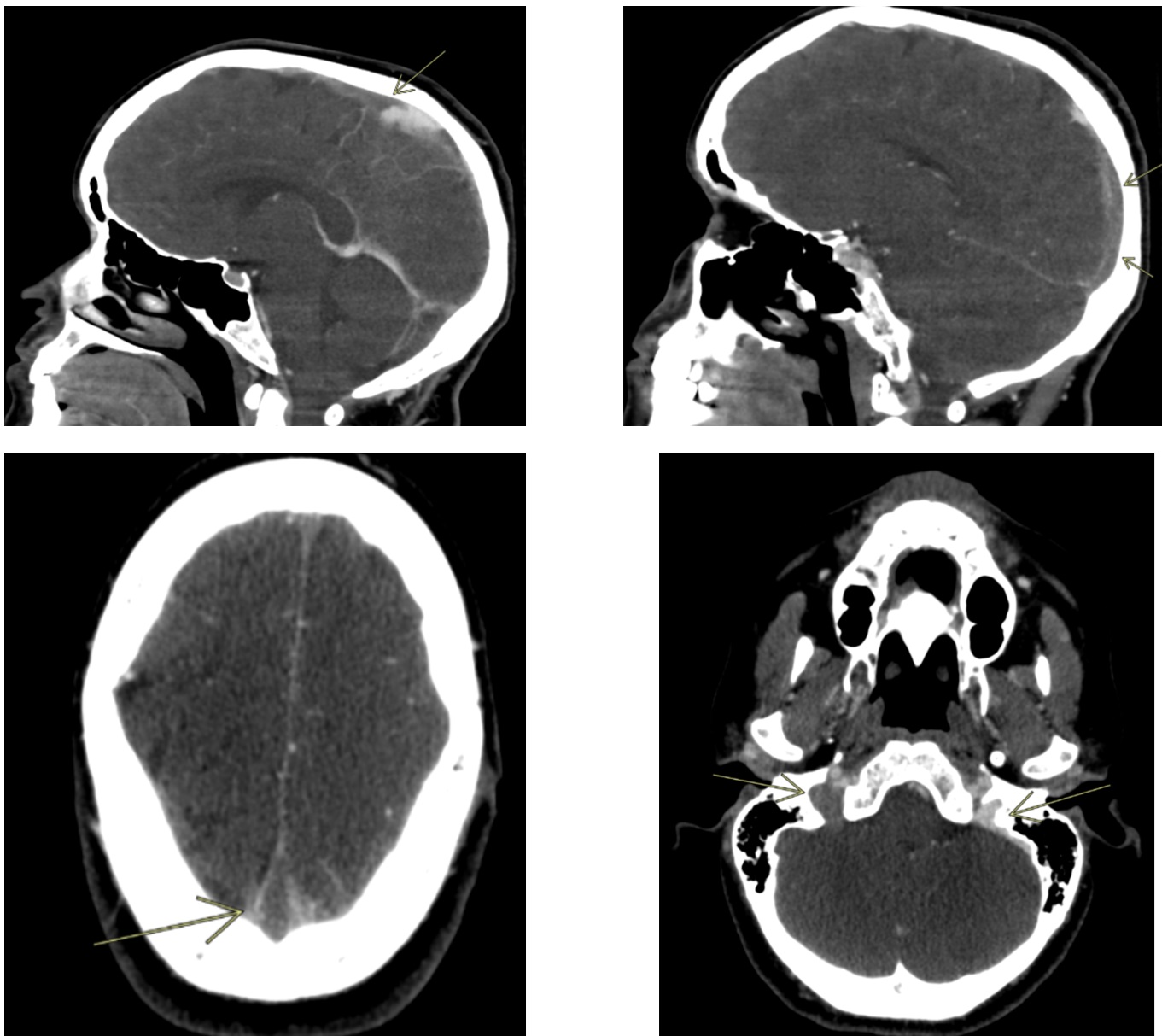
Initial imaging studies revealed extensive CVT involving major venous sinuses, particularly the superior sagittal sinus. Urgent thrombectomy resulted in full recanalization of the affected sinuses. Follow-up MRI revealed an acute infarct in the left frontal lobe with a hemorrhagic component. Further workup, including a colonoscopy, revealed mild to moderate chronic ulcerative pancolitis. An acute UC flare in the setting of recent OCP use was determined to be the most likely cause of the patient's hypercoagulability.
Management involved a multidisciplinary approach with anticoagulation therapy initiated via a heparin drip, transitioning to warfarin, and then Eliquis upon discharge. Prednisone was initiated for UC management, with plans to start biologics as an outpatient. Keppra was also administered for seizure prophylaxis. The patient showed notable improvement and was discharged with follow-up plans in place.
Discussion: CVT is a rare extraintestinal manifestation of IBD that requires high clinical suspicion, especially in patients presenting with neurological symptoms and a history suggestive of UC. This case emphasizes the importance of multidisciplinary management and advanced imaging techniques for accurate diagnosis. The literature review underscores the significant epidemiological association between IBD and increased risk of CVT, the complex pathophysiological mechanisms linking IBD to thrombotic events, and the multifaceted treatment strategies required for optimal patient outcomes.
Disclosures:
Abakar Baraka, MD1, Benjamin Heriford, DO2, Jawairia Memon, MD3, Diego Cebrian, MD4. P4405 - Cerebral Venous Thrombosis as an Initial Presentation of Ulcerative Colitis: A Case Report and Literature Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Colorado-Anschutz Campus, San Antonio, TX; 2UTHSCSA, San Antonio, TX; 3University of Texas Health Science Center, San Antonio, TX; 4University of Texas Health San Antonio, San Antonio, TX
Introduction: Cerebral venous thrombosis (CVT) is a rare but significant neurological condition often leading to severe complications such as stroke. While CVT can result from various etiologies, its association with systemic inflammatory diseases like inflammatory bowel disease (IBD), particularly ulcerative colitis (UC), has garnered increasing clinical attention. This case report explores CVT as an initial extraintestinal manifestation of UC, highlighting the diagnostic challenges and the need for considering IBD in the differential diagnosis of CVT.
Case Description/Methods: A 26-year-old female with no significant past medical history, aside from oral contraceptive pill use, presented with recent gastrointestinal symptoms characterized by diarrhea with intermittent hematochezia and melena. Her symptoms progressed over several weeks, eventually leading to severe headaches, right-sided weakness, and dysarthria. Acute neurological decline manifested as seizures, prompting urgent medical attention.
Initial imaging studies revealed extensive CVT involving major venous sinuses, particularly the superior sagittal sinus. Urgent thrombectomy resulted in full recanalization of the affected sinuses. Follow-up MRI revealed an acute infarct in the left frontal lobe with a hemorrhagic component. Further workup, including a colonoscopy, revealed mild to moderate chronic ulcerative pancolitis. An acute UC flare in the setting of recent OCP use was determined to be the most likely cause of the patient's hypercoagulability.
Management involved a multidisciplinary approach with anticoagulation therapy initiated via a heparin drip, transitioning to warfarin, and then Eliquis upon discharge. Prednisone was initiated for UC management, with plans to start biologics as an outpatient. Keppra was also administered for seizure prophylaxis. The patient showed notable improvement and was discharged with follow-up plans in place.
Discussion: CVT is a rare extraintestinal manifestation of IBD that requires high clinical suspicion, especially in patients presenting with neurological symptoms and a history suggestive of UC. This case emphasizes the importance of multidisciplinary management and advanced imaging techniques for accurate diagnosis. The literature review underscores the significant epidemiological association between IBD and increased risk of CVT, the complex pathophysiological mechanisms linking IBD to thrombotic events, and the multifaceted treatment strategies required for optimal patient outcomes.
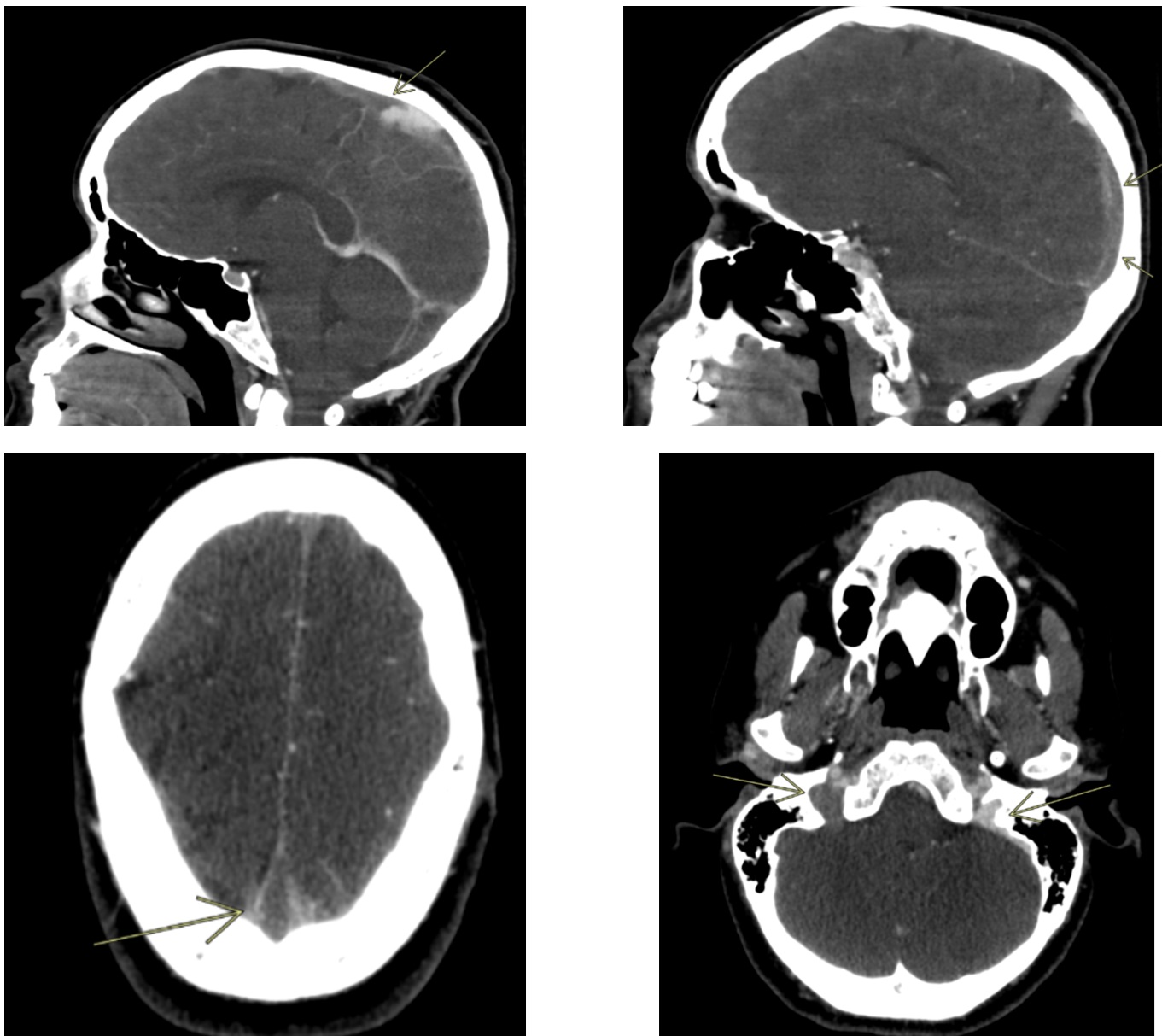
Figure: CT Head showing extensive cerebral venous thrombosis with involvement of the superior sagittal sinus and thrombus extension into the right transverse sinus, sigmoid sinus, and proximal internal jugular vein
Disclosures:
Abakar Baraka indicated no relevant financial relationships.
Benjamin Heriford indicated no relevant financial relationships.
Jawairia Memon indicated no relevant financial relationships.
Diego Cebrian indicated no relevant financial relationships.
Abakar Baraka, MD1, Benjamin Heriford, DO2, Jawairia Memon, MD3, Diego Cebrian, MD4. P4405 - Cerebral Venous Thrombosis as an Initial Presentation of Ulcerative Colitis: A Case Report and Literature Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
