Tuesday Poster Session
Category: IBD
P4411 - De Novo Ulcerative Colitis in a Patient with Rapidly Progressive Glomerulonephritis (RPGN) after Renal Transplant
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Qumber Ali, DO
University of Arizona College of Medicine
Phoenix, AZ
Presenting Author(s)
Qumber Ali, DO1, Rohit Khanna, DO2, Joy-Marie Hermes, MD3, Olivia Lanser, MD2, Jonathan Fisher, MD4, James Rice, MD4, Gauree Konijetti, MD4
1University of Arizona College of Medicine, Phoenix, AZ; 2Scripps Green Hospital, San Diego, CA; 3Scripps Clinic & Scripps Research Institute, San Diego, CA; 4Scripps Clinic, San Diego, CA
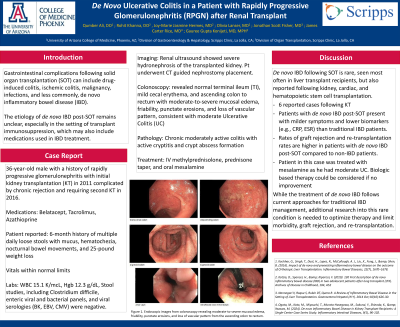
Introduction: Gastrointestinal complications following solid organ transplantation (SOT) can include drug-induced colitis, ischemic colitis, malignancy, infections, and less commonly, de novo inflammatory bowel disease (IBD). The etiology of de novo IBD post-SOT remains unclear, especially in the setting of transplant immunosuppression, which may also include medications used in IBD treatment. This case discusses a new diagnosis of ulcerative colitis (UC) in a patient with a history of kidney transplant.
Case Description/Methods: Patient is a 36-year-old male with a history of rapidly progressive glomerulonephritis with initial kidney transplantation (KT) in 2011 complicated by chronic rejection and requiring second KT in 2016. Current medications include belatacept, tacrolimus, and azathioprine. Patient reported a 6-month history of multiple daily loose stools with mucus, hematochezia, nocturnal bowel movements, and a 25-pound weight loss. Vital signs were normal. Labs revealed WBC 15.1 K/mcL and hemoglobin 12.3 g/dL. Stool studies, including Clostridium difficile, enteric viral and bacterial panels, and viral serologies (BK, EBV, CMV) were negative. A renal ultrasound showed severe hydronephrosis of the transplanted kidney, requiring CT guided nephrostomy placement. Colonoscopy showed a normal terminal ileum (TI), mild cecal erythema, and ascending colon to rectum with moderate-to-severe mucosal edema, friability, punctate erosions, and loss of vascular pattern, consistent with moderate UC pancolitis. Histopathology revealed a normal TI and chronic moderately active colitis with active cryptitis and crypt abscess formation. Patient was started on IV methylprednisolone, which provided symptomatic relief, and ultimately discharged on a prednisone taper and oral mesalamine.
Discussion: De novo IBD following SOT is rare, seen most often in liver transplant recipients, but also reported following kidney, cardiac, and hematopoietic stem cell transplantation. To date, there are only 6 reported cases following KT. Patients with de novo IBD post-SOT present with milder symptoms and lower biomarkers (e.g., CRP, ESR) than traditional IBD patients. However, rates of graft rejection and re-transplantation rates are higher in patients with de novo IBD post-SOT compared to non-IBD patients. While the treatment of de novo IBD follows current approaches for traditional IBD management, additional research into this rare condition is needed to optimize therapy and limit morbidity, graft rejection, and re-transplantation.
Disclosures:
Qumber Ali, DO1, Rohit Khanna, DO2, Joy-Marie Hermes, MD3, Olivia Lanser, MD2, Jonathan Fisher, MD4, James Rice, MD4, Gauree Konijetti, MD4. P4411 - De Novo Ulcerative Colitis in a Patient with Rapidly Progressive Glomerulonephritis (RPGN) after Renal Transplant, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Arizona College of Medicine, Phoenix, AZ; 2Scripps Green Hospital, San Diego, CA; 3Scripps Clinic & Scripps Research Institute, San Diego, CA; 4Scripps Clinic, San Diego, CA
Introduction: Gastrointestinal complications following solid organ transplantation (SOT) can include drug-induced colitis, ischemic colitis, malignancy, infections, and less commonly, de novo inflammatory bowel disease (IBD). The etiology of de novo IBD post-SOT remains unclear, especially in the setting of transplant immunosuppression, which may also include medications used in IBD treatment. This case discusses a new diagnosis of ulcerative colitis (UC) in a patient with a history of kidney transplant.
Case Description/Methods: Patient is a 36-year-old male with a history of rapidly progressive glomerulonephritis with initial kidney transplantation (KT) in 2011 complicated by chronic rejection and requiring second KT in 2016. Current medications include belatacept, tacrolimus, and azathioprine. Patient reported a 6-month history of multiple daily loose stools with mucus, hematochezia, nocturnal bowel movements, and a 25-pound weight loss. Vital signs were normal. Labs revealed WBC 15.1 K/mcL and hemoglobin 12.3 g/dL. Stool studies, including Clostridium difficile, enteric viral and bacterial panels, and viral serologies (BK, EBV, CMV) were negative. A renal ultrasound showed severe hydronephrosis of the transplanted kidney, requiring CT guided nephrostomy placement. Colonoscopy showed a normal terminal ileum (TI), mild cecal erythema, and ascending colon to rectum with moderate-to-severe mucosal edema, friability, punctate erosions, and loss of vascular pattern, consistent with moderate UC pancolitis. Histopathology revealed a normal TI and chronic moderately active colitis with active cryptitis and crypt abscess formation. Patient was started on IV methylprednisolone, which provided symptomatic relief, and ultimately discharged on a prednisone taper and oral mesalamine.
Discussion: De novo IBD following SOT is rare, seen most often in liver transplant recipients, but also reported following kidney, cardiac, and hematopoietic stem cell transplantation. To date, there are only 6 reported cases following KT. Patients with de novo IBD post-SOT present with milder symptoms and lower biomarkers (e.g., CRP, ESR) than traditional IBD patients. However, rates of graft rejection and re-transplantation rates are higher in patients with de novo IBD post-SOT compared to non-IBD patients. While the treatment of de novo IBD follows current approaches for traditional IBD management, additional research into this rare condition is needed to optimize therapy and limit morbidity, graft rejection, and re-transplantation.
Disclosures:
Qumber Ali indicated no relevant financial relationships.
Rohit Khanna indicated no relevant financial relationships.
Joy-Marie Hermes indicated no relevant financial relationships.
Olivia Lanser indicated no relevant financial relationships.
Jonathan Fisher indicated no relevant financial relationships.
James Rice indicated no relevant financial relationships.
Gauree Konijetti indicated no relevant financial relationships.
Qumber Ali, DO1, Rohit Khanna, DO2, Joy-Marie Hermes, MD3, Olivia Lanser, MD2, Jonathan Fisher, MD4, James Rice, MD4, Gauree Konijetti, MD4. P4411 - De Novo Ulcerative Colitis in a Patient with Rapidly Progressive Glomerulonephritis (RPGN) after Renal Transplant, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
