Tuesday Poster Session
Category: IBD
P4413 - Mimicry and Deception in CMUSE
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Naveena Luke, MD
NYU Langone Health
New York, NY
Presenting Author(s)
Naveena Luke, MD1, Seymour Katz, MD2
1NYU Langone Health, New York, NY; 2NYU Grossman School of Medicine, New Hyde Park, NY
Introduction: Cryptogenic multifocal ulcerating stenosing enteritis (CMUSE) is a rare, perplexing, and underdiagnosed disease within the realm of inflammatory bowel diseases (IBDs). Its cryptic nature is marked by a constellation of symptoms reminiscent of more common gastrointestinal disorders. In this case report, we present a case of CMUSE, highlighting the complexity of its clinical presentation and the therapeutic considerations that underscore its enigmatic character.
Case Description/Methods: A 41-year-old patient is being followed for recurrent melena and chronic blood loss anemia, fatigue, and intermittent abdominal over the course of several years. Initial endoscopic workup was nondiagnostic, however index capsule endoscopy revealed ulcerations throughout the small bowel, thought to be due to Crohn’s. The patient trialed biologic therapy including Humeira, Remicade, and Stelara with persistent symptoms, including obstruction. Diagnostic laparoscopy was converted to an open small bowel resection due to the presence of complex adhesions and sequential strictured segments of enteritis. The pathology report indicated ulcerations in the small intestine extending as deep as the muscularis propria, without granulomas, compatible with a diagnosis of CMUSE. He has since undergone two additional bowel resections. The intervening mucosa appeared normal, and microscopically, the villous architecture was preserved. No active or chronic enteritis, granuloma, or vascular abnormalities were seen. Post operatively, he only temporarily had improvement of symptoms.
Discussion: CMUSE can be distinguished by its unique pathology, such as the presence of superficial, discrete ulcers and strictures in the small intestine, which are not typical of other IBDs. Other features of CMUSE include relapsing or chronic ulcerative stenosis after resection, no signs of systemic inflammation, and no penetrating disease. Use of steroids has had mixed efficacy and biologics are typically unsuccessful. In patients who undergo surgery, majority have recurrence. Due to the rarity of CMUSE and its enigmatic etiology, there are no specific, targeted treatments available. Management is largely guided by empirical therapeutic strategies and palliative interventions. The lack of well-defined diagnostic criteria and an incomplete understanding of its underlying pathogenesis further underscore the imperative for case documentations, further research, and heightened awareness among clinicians to better understand and manage this condition.

Disclosures:
Naveena Luke, MD1, Seymour Katz, MD2. P4413 - Mimicry and Deception in CMUSE, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1NYU Langone Health, New York, NY; 2NYU Grossman School of Medicine, New Hyde Park, NY
Introduction: Cryptogenic multifocal ulcerating stenosing enteritis (CMUSE) is a rare, perplexing, and underdiagnosed disease within the realm of inflammatory bowel diseases (IBDs). Its cryptic nature is marked by a constellation of symptoms reminiscent of more common gastrointestinal disorders. In this case report, we present a case of CMUSE, highlighting the complexity of its clinical presentation and the therapeutic considerations that underscore its enigmatic character.
Case Description/Methods: A 41-year-old patient is being followed for recurrent melena and chronic blood loss anemia, fatigue, and intermittent abdominal over the course of several years. Initial endoscopic workup was nondiagnostic, however index capsule endoscopy revealed ulcerations throughout the small bowel, thought to be due to Crohn’s. The patient trialed biologic therapy including Humeira, Remicade, and Stelara with persistent symptoms, including obstruction. Diagnostic laparoscopy was converted to an open small bowel resection due to the presence of complex adhesions and sequential strictured segments of enteritis. The pathology report indicated ulcerations in the small intestine extending as deep as the muscularis propria, without granulomas, compatible with a diagnosis of CMUSE. He has since undergone two additional bowel resections. The intervening mucosa appeared normal, and microscopically, the villous architecture was preserved. No active or chronic enteritis, granuloma, or vascular abnormalities were seen. Post operatively, he only temporarily had improvement of symptoms.
Discussion: CMUSE can be distinguished by its unique pathology, such as the presence of superficial, discrete ulcers and strictures in the small intestine, which are not typical of other IBDs. Other features of CMUSE include relapsing or chronic ulcerative stenosis after resection, no signs of systemic inflammation, and no penetrating disease. Use of steroids has had mixed efficacy and biologics are typically unsuccessful. In patients who undergo surgery, majority have recurrence. Due to the rarity of CMUSE and its enigmatic etiology, there are no specific, targeted treatments available. Management is largely guided by empirical therapeutic strategies and palliative interventions. The lack of well-defined diagnostic criteria and an incomplete understanding of its underlying pathogenesis further underscore the imperative for case documentations, further research, and heightened awareness among clinicians to better understand and manage this condition.

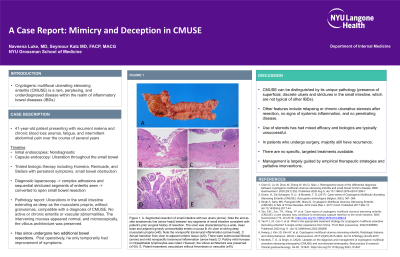
Figure: Figure 1. A. Segmental resection of small intestine with two ulcers (arrow). Note the end-to-side anastomotic line (arrow head) between two segments of small intestine consistent with patient’s prior surgical history of resection. The ulcer was characterized by a wide, clean base and adjacent grossly unremarkable enteric mucosa B. An ulcer involving deep muscularis propria (x40). Note the nonspecific transmural inflammation (arrow head). C. Abrupt transition from ulcer to adjacent enteric tissue (x20). There were submucosal fibrosis (arrow) and mild nonspecific transmural inflammation (arrow head). D. Patchy mild increase in intraepithelial lymphocytes was noted. However, the villous architecture was preserved (x100). E. Patent mesenteric vasculature without thrombosis or vasculitis (x40).
Disclosures:
Naveena Luke indicated no relevant financial relationships.
Seymour Katz indicated no relevant financial relationships.
Naveena Luke, MD1, Seymour Katz, MD2. P4413 - Mimicry and Deception in CMUSE, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

