Tuesday Poster Session
Category: IBD
P4414 - A Multidisciplinary Approach to Fungemia During an Acute Crohn's Flare
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- ES
Elisha Shah, DO
Baystate Medical Center
Springfield, MA
Presenting Author(s)
Elisha Shah, DO1, Victoria Caruso, DO1, Yesenia Greeff, MD2
1Baystate Medical Center, Springfield, MA; 2University of Massachusetts Chan Medical School - Baystate, Springfield, MA
Introduction: Fungemia can be a life-threatening complication for any patient. For patients with severe active Crohn's disease, this type of complication, though rare, can lead to immensely complex decision-making. We present a clinical conundrum faced while treating a patient with concomitant fungemia and Crohn’s flare.
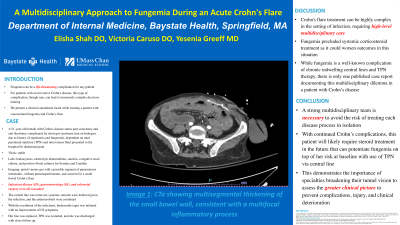
Case Description/Methods: A 51-year-old female with Crohn's disease status post colectomy and end ileostomy complicated by short gut syndrome (not on biologics due to history of septicemia and fungemia), dependent on total parenteral nutrition (TPN) and intravenous fluid presented to the hospital for abdominal pain. Vitals were stable and labs revealed leukocytosis, electrolyte abnormalities, anemia, a negative stool culture, and positive blood cultures for Serratia and Candida. Imaging revealed portal venous gas with a possible segment of pneumatosis intestinalis, without pneumoperitoneum, and concern for a small bowel Crohn’s flare. Infectious disease (ID), gastroenterology (GI), and colorectal surgery were all consulted. The central line was removed, systemic steroids were deferred given the infection, and the antimicrobials were continued. With the resolution of the infections, budesonide taper was initiated with an improvement of GI symptoms. Her line was replaced, TPN was restarted, and she was discharged with close follow-up with ID and GI.
Discussion: Crohn's flare treatment can be highly complex in the setting of infection, requiring high-level multidisciplinary care. Fungemia precluded systemic corticosteroid treatment as it could worsen outcomes in this situation. While fungemia is a well-known complication of chronic indwelling central lines and TPN therapy, there is only one published case report documenting this multidisciplinary dilemma in a patient with Crohn’s disease. A strong multidisciplinary team is necessary to avoid the risk of treating each disease process in isolation. With continued Crohn’s complications, this patient will likely require steroid treatment in the future that can potentiate fungemia on top of her risk at baseline with the use of TPN via central line. This demonstrates the importance of specialties broadening their tunnel vision to assess the greater clinical picture to prevent complications, injury, and clinical deterioration.
Disclosures:
Elisha Shah, DO1, Victoria Caruso, DO1, Yesenia Greeff, MD2. P4414 - A Multidisciplinary Approach to Fungemia During an Acute Crohn's Flare, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Baystate Medical Center, Springfield, MA; 2University of Massachusetts Chan Medical School - Baystate, Springfield, MA
Introduction: Fungemia can be a life-threatening complication for any patient. For patients with severe active Crohn's disease, this type of complication, though rare, can lead to immensely complex decision-making. We present a clinical conundrum faced while treating a patient with concomitant fungemia and Crohn’s flare.
Case Description/Methods: A 51-year-old female with Crohn's disease status post colectomy and end ileostomy complicated by short gut syndrome (not on biologics due to history of septicemia and fungemia), dependent on total parenteral nutrition (TPN) and intravenous fluid presented to the hospital for abdominal pain. Vitals were stable and labs revealed leukocytosis, electrolyte abnormalities, anemia, a negative stool culture, and positive blood cultures for Serratia and Candida. Imaging revealed portal venous gas with a possible segment of pneumatosis intestinalis, without pneumoperitoneum, and concern for a small bowel Crohn’s flare. Infectious disease (ID), gastroenterology (GI), and colorectal surgery were all consulted. The central line was removed, systemic steroids were deferred given the infection, and the antimicrobials were continued. With the resolution of the infections, budesonide taper was initiated with an improvement of GI symptoms. Her line was replaced, TPN was restarted, and she was discharged with close follow-up with ID and GI.
Discussion: Crohn's flare treatment can be highly complex in the setting of infection, requiring high-level multidisciplinary care. Fungemia precluded systemic corticosteroid treatment as it could worsen outcomes in this situation. While fungemia is a well-known complication of chronic indwelling central lines and TPN therapy, there is only one published case report documenting this multidisciplinary dilemma in a patient with Crohn’s disease. A strong multidisciplinary team is necessary to avoid the risk of treating each disease process in isolation. With continued Crohn’s complications, this patient will likely require steroid treatment in the future that can potentiate fungemia on top of her risk at baseline with the use of TPN via central line. This demonstrates the importance of specialties broadening their tunnel vision to assess the greater clinical picture to prevent complications, injury, and clinical deterioration.
Disclosures:
Elisha Shah indicated no relevant financial relationships.
Victoria Caruso indicated no relevant financial relationships.
Yesenia Greeff indicated no relevant financial relationships.
Elisha Shah, DO1, Victoria Caruso, DO1, Yesenia Greeff, MD2. P4414 - A Multidisciplinary Approach to Fungemia During an Acute Crohn's Flare, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
