Tuesday Poster Session
Category: IBD
P4419 - Gut on Fire: Immune Checkpoint Inhibitor-Induced Gastrointestinal Inflammation
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ahmad Mardini, MD
Advocate Christ Medical Center
Oak Lawn, IL
Presenting Author(s)
Ahmad Mardini, MD, Samee Farooqi, DO, Matthew Posen, DO, Krishna Shah, MD, Harreth Raddawi, MD
Advocate Christ Medical Center, Oak Lawn, IL
Introduction: Immune checkpoint inhibitors help treat cancers. Their side effects, called immune-related adverse events have been reported. While immune checkpoint inhibitor colitis is recognized, immune checkpoint inhibitor celiac disease is rarely identified. Even rarer is gastritis. We present a case of ipilimumab induced colitis, celiac disease and gastritis.
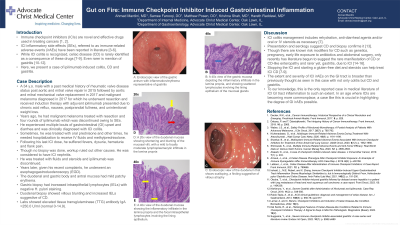
Case Description/Methods: A 34 year old male with a history of previous malignant melanoma presented due to chronic acid reflux, nausea, postprandial fullness, and unintentional weight loss. Years ago, the melanoma was treated with resection and four rounds of ipilimumab. He experienced multiple bouts of gastrointestinal upset and diarrhea and was clinically diagnosed with immune checkpoint inhibitor colitis. Sometimes, he was treated with oral prednisone. Other times, he was hospitalized to receive fluids and methylprednisolone. Following his last ipilimumab dose, he had fevers, dysuria, hematuria and flank pain. No biopsy was done but workup ruled out other causes. He was considered to have immune checkpoint inhibitor nephritis. Ipilimumab was discontinued. Years later, given his recent complaints, he underwent an esophagogastroduodenoscopy. The duodenal and gastric body and antral mucosa had mild patchy erythema. Gastric biopsy had increased intraepithelial lymphocytes with negative H. pylori staining. Duodenal biopsy showed villous blunting and increased intraepithelial lymphocytes. Labs showed elevated tissue transglutaminase antibody immunoglobulin A >250.0 U/ml (normal 0-14.9).
Discussion: Immune checkpoint inhibitor colitis management includes rehydration, anti-diarrheal agents and/or steroids as necessary. Presentation and serology suggest celiac disease and biopsy confirms it. Risk modifiers for celiac disease are known, but only recently has literature begun to suggest the rare manifestation of celiac disease and rarer yet, gastritis, due to immune checkpoint inhibitors. Stopping the inhibitor and starting a gluten-free diet and steroids can help treat immune checkpoint inhibitor celiac disease. The extent and severity of immune checkpoint inhibitor immune-related adverse events on the gastrointestinal tract is broader than previously thought. To our knowledge, this is the only reported case in literature of immune checkpoint inhibitor gastrointestinal tract inflammation of such an extent. In an age where these drugs are becoming commonplace, this case is crucial in highlighting the degree of gastrointestinal side effects possible.
Disclosures:
Ahmad Mardini, MD, Samee Farooqi, DO, Matthew Posen, DO, Krishna Shah, MD, Harreth Raddawi, MD. P4419 - Gut on Fire: Immune Checkpoint Inhibitor-Induced Gastrointestinal Inflammation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Advocate Christ Medical Center, Oak Lawn, IL
Introduction: Immune checkpoint inhibitors help treat cancers. Their side effects, called immune-related adverse events have been reported. While immune checkpoint inhibitor colitis is recognized, immune checkpoint inhibitor celiac disease is rarely identified. Even rarer is gastritis. We present a case of ipilimumab induced colitis, celiac disease and gastritis.
Case Description/Methods: A 34 year old male with a history of previous malignant melanoma presented due to chronic acid reflux, nausea, postprandial fullness, and unintentional weight loss. Years ago, the melanoma was treated with resection and four rounds of ipilimumab. He experienced multiple bouts of gastrointestinal upset and diarrhea and was clinically diagnosed with immune checkpoint inhibitor colitis. Sometimes, he was treated with oral prednisone. Other times, he was hospitalized to receive fluids and methylprednisolone. Following his last ipilimumab dose, he had fevers, dysuria, hematuria and flank pain. No biopsy was done but workup ruled out other causes. He was considered to have immune checkpoint inhibitor nephritis. Ipilimumab was discontinued. Years later, given his recent complaints, he underwent an esophagogastroduodenoscopy. The duodenal and gastric body and antral mucosa had mild patchy erythema. Gastric biopsy had increased intraepithelial lymphocytes with negative H. pylori staining. Duodenal biopsy showed villous blunting and increased intraepithelial lymphocytes. Labs showed elevated tissue transglutaminase antibody immunoglobulin A >250.0 U/ml (normal 0-14.9).
Discussion: Immune checkpoint inhibitor colitis management includes rehydration, anti-diarrheal agents and/or steroids as necessary. Presentation and serology suggest celiac disease and biopsy confirms it. Risk modifiers for celiac disease are known, but only recently has literature begun to suggest the rare manifestation of celiac disease and rarer yet, gastritis, due to immune checkpoint inhibitors. Stopping the inhibitor and starting a gluten-free diet and steroids can help treat immune checkpoint inhibitor celiac disease. The extent and severity of immune checkpoint inhibitor immune-related adverse events on the gastrointestinal tract is broader than previously thought. To our knowledge, this is the only reported case in literature of immune checkpoint inhibitor gastrointestinal tract inflammation of such an extent. In an age where these drugs are becoming commonplace, this case is crucial in highlighting the degree of gastrointestinal side effects possible.
Figure: A: Endoscopic view of the gastric antrum with inflammation/erythema representative of gastritis.
B: A 40x view of the gastric mucosa depicting the inflammatory infiltrate in the lamina propria, and showing scattered lymphocytes involving the lining epithelium of the mucosal glands.
C: Endoscopic view of the duodenum that shows scalloping, a finding suggestive of villous atrophy.
D: A 20x view of the duodenal mucosa showing shortening and blunting of the mucosal villi, with a mild to focally moderate lymphoplasmacytic infiltrate in the lamina propria.
E: A 40x view of the duodenal mucosa showing the inflammatory infiltrate in the lamina propria and the focal intraepithelial lymphocytes involving the lining epithelium.
B: A 40x view of the gastric mucosa depicting the inflammatory infiltrate in the lamina propria, and showing scattered lymphocytes involving the lining epithelium of the mucosal glands.
C: Endoscopic view of the duodenum that shows scalloping, a finding suggestive of villous atrophy.
D: A 20x view of the duodenal mucosa showing shortening and blunting of the mucosal villi, with a mild to focally moderate lymphoplasmacytic infiltrate in the lamina propria.
E: A 40x view of the duodenal mucosa showing the inflammatory infiltrate in the lamina propria and the focal intraepithelial lymphocytes involving the lining epithelium.
Disclosures:
Ahmad Mardini indicated no relevant financial relationships.
Samee Farooqi indicated no relevant financial relationships.
Matthew Posen indicated no relevant financial relationships.
Krishna Shah indicated no relevant financial relationships.
Harreth Raddawi indicated no relevant financial relationships.
Ahmad Mardini, MD, Samee Farooqi, DO, Matthew Posen, DO, Krishna Shah, MD, Harreth Raddawi, MD. P4419 - Gut on Fire: Immune Checkpoint Inhibitor-Induced Gastrointestinal Inflammation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
