Tuesday Poster Session
Category: IBD
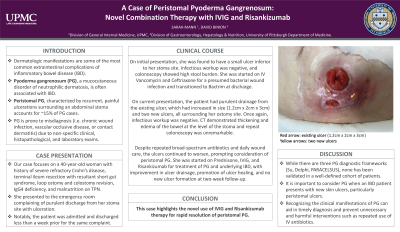
P4447 - A Case of Peristomal PG: Novel Combination Therapy With IVIG and Risankizumab
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Sarah Mann, MD
University of Pittsburgh Medical Center
Pittsburgh, PA
Presenting Author(s)
Award: Presidential Poster Award
Sarah Mann, MD, David Binion, MD
University of Pittsburgh Medical Center, Pittsburgh, PA
Introduction: Dermatologic manifestations are some of the most common extraintestinal complications of inflammatory bowel disease (IBD). Pyoderma gangrenosum (PG), a mucocutaneous disorder of neutrophilic dermatosis, is often associated with IBD. Peristomal PG, characterized by recurrent, painful ulcerations surrounding an abdominal stoma, accounts for ~15% of PG cases. PG is prone to misdiagnosis due to non-specific clinical, histopathological, and laboratory exams.
Case Description/Methods: A 40-year-old woman with history of severe refractory Crohn’s disease, terminal ileum resection with resultant short gut syndrome, loop ostomy and colostomy revision, IgG4 deficiency, and malnutrition on total parenteral nutrition, presented to the hospital complaining of purulent discharge from her stoma site with ulceration.
The patient was admitted and discharged less than a week prior to the current presentation for the same chief complaint where she was found to have a small ulcer inferior to her stoma site. Infectious workup was negative, and colonoscopy showed high stool burden. She was started on IV Vancomycin and Ceftriaxone for a presumed bacterial wound infection and transitioned to Bactrim on discharge.
On current presentation, the patient had purulent drainage from the existing ulcer, which had increased in size (1.2 cm x 2 cm x 3 cm) and two new ulcers, all surrounding her ostomy site. Infectious workup was negative. CT abdomen/pelvis showed thickening and edema of the bowel at the level of the stoma, and colonoscopy was unremarkable. Despite repeated broad-spectrum antibiotics and daily wound care, the ulcers continued to worsen, prompting consideration for peristomal PG. She was started on Prednisone, IVIG, and Risankizumab for treatment of PG and underlying IBD, with improvement in ulcer drainage, promotion of ulcer healing, and no new ulcer formation.
Discussion: PG is often misdiagnosed as a chronic wound infection, vascular occlusive disease, or contact dermatitis. While there are three PG diagnostic frameworks (Su, Delphi, PARACELSUS), none has been validated in a well-defined cohort of patients. It is important to consider PG when an IBD patient presents with new skin ulcers, particularly peristomal ulcers. Recognizing the clinical manifestations of PG can aid in timely diagnosis and prevent unnecessary and harmful interventions such as repeated use of IV antibiotics. Furthermore, this case highlights the novel use of IVIG and Risankizumab combination therapy for rapid resolution of peristomal PG.
Disclosures:
Sarah Mann, MD, David Binion, MD. P4447 - A Case of Peristomal PG: Novel Combination Therapy With IVIG and Risankizumab, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Sarah Mann, MD, David Binion, MD
University of Pittsburgh Medical Center, Pittsburgh, PA
Introduction: Dermatologic manifestations are some of the most common extraintestinal complications of inflammatory bowel disease (IBD). Pyoderma gangrenosum (PG), a mucocutaneous disorder of neutrophilic dermatosis, is often associated with IBD. Peristomal PG, characterized by recurrent, painful ulcerations surrounding an abdominal stoma, accounts for ~15% of PG cases. PG is prone to misdiagnosis due to non-specific clinical, histopathological, and laboratory exams.
Case Description/Methods: A 40-year-old woman with history of severe refractory Crohn’s disease, terminal ileum resection with resultant short gut syndrome, loop ostomy and colostomy revision, IgG4 deficiency, and malnutrition on total parenteral nutrition, presented to the hospital complaining of purulent discharge from her stoma site with ulceration.
The patient was admitted and discharged less than a week prior to the current presentation for the same chief complaint where she was found to have a small ulcer inferior to her stoma site. Infectious workup was negative, and colonoscopy showed high stool burden. She was started on IV Vancomycin and Ceftriaxone for a presumed bacterial wound infection and transitioned to Bactrim on discharge.
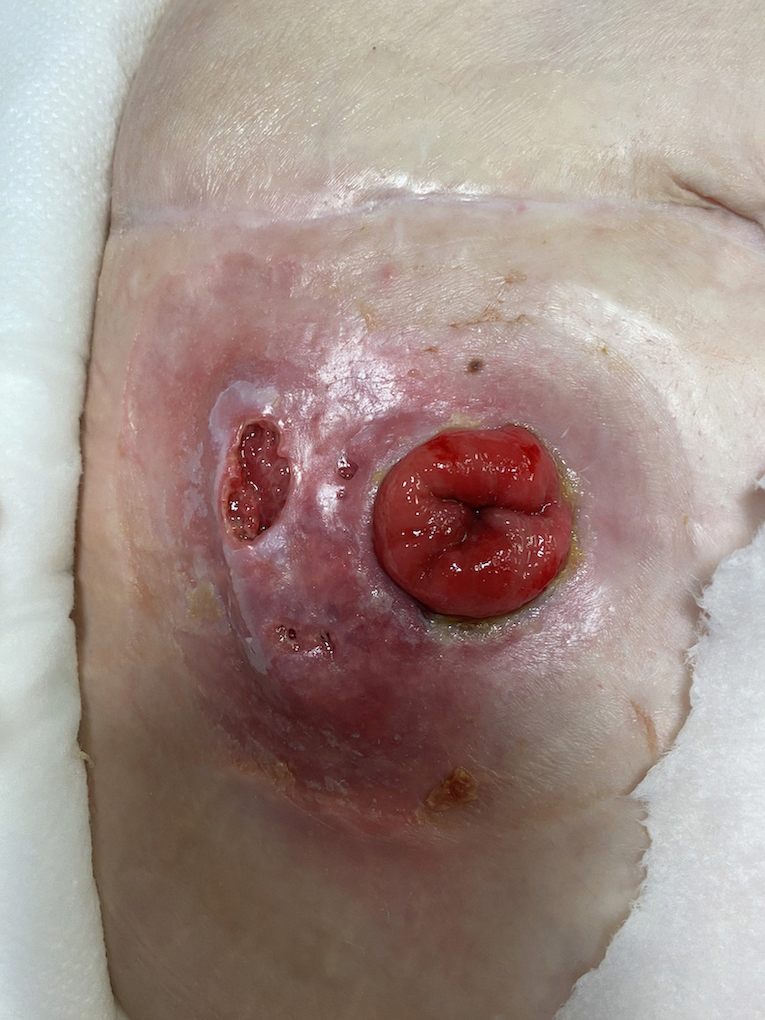
On current presentation, the patient had purulent drainage from the existing ulcer, which had increased in size (1.2 cm x 2 cm x 3 cm) and two new ulcers, all surrounding her ostomy site. Infectious workup was negative. CT abdomen/pelvis showed thickening and edema of the bowel at the level of the stoma, and colonoscopy was unremarkable. Despite repeated broad-spectrum antibiotics and daily wound care, the ulcers continued to worsen, prompting consideration for peristomal PG. She was started on Prednisone, IVIG, and Risankizumab for treatment of PG and underlying IBD, with improvement in ulcer drainage, promotion of ulcer healing, and no new ulcer formation.
Discussion: PG is often misdiagnosed as a chronic wound infection, vascular occlusive disease, or contact dermatitis. While there are three PG diagnostic frameworks (Su, Delphi, PARACELSUS), none has been validated in a well-defined cohort of patients. It is important to consider PG when an IBD patient presents with new skin ulcers, particularly peristomal ulcers. Recognizing the clinical manifestations of PG can aid in timely diagnosis and prevent unnecessary and harmful interventions such as repeated use of IV antibiotics. Furthermore, this case highlights the novel use of IVIG and Risankizumab combination therapy for rapid resolution of peristomal PG.
Figure: Peristomal ulcer (1.2 cm x 2 cm x 3 cm)
Disclosures:
Sarah Mann indicated no relevant financial relationships.
David Binion indicated no relevant financial relationships.
Sarah Mann, MD, David Binion, MD. P4447 - A Case of Peristomal PG: Novel Combination Therapy With IVIG and Risankizumab, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

