Tuesday Poster Session
Category: IBD
P4451 - Evan’s Syndrome in a Patient With Ulcerative Colitis: A Rare Extraintestinal Manifestation
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
.jpg)
Erica Graff, MD
University Hospitals Cleveland Medical Center, Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Erica Graff, MD1, Jenny Jan, MD2, Jeffry Katz, MD3, Vu Q. Nguyen, MD, MS3
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2University Hospitals Cleveland Medical Center, Cleveland, OH; 3Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: Inflammatory bowel disease (IBD) is an autoimmune condition affecting the gastrointestinal tract that can also affect other organ systems. Over 50% of patients with IBD develop extraintestinal manifestations (EIMs), with hematologic EIMs being less common. We present a rare case of a patient with ulcerative colitis and concurrent Evan’s syndrome.
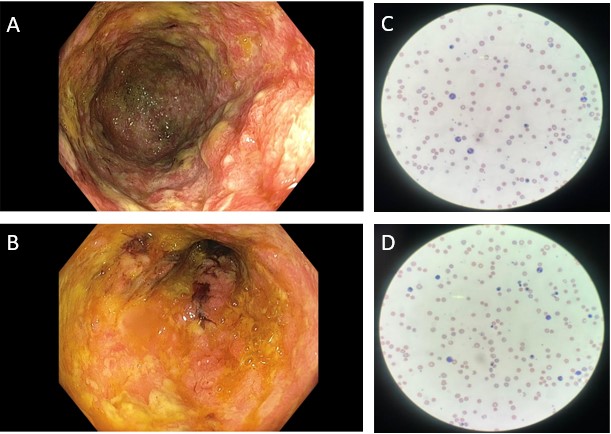
Case Description/Methods: A 44 year-old previously healthy man presented to gastroenterology clinic with more than ten loose, bloody and watery stools daily for the last 2 months. He also had bloating, tenesmus and a 10-pound weight loss over six months. He was pale on physical exam, with labs notable for a hemoglobin of 5 g/dL. He was admitted to the hospital for expedited work-up where colonoscopy showed Mayo 3 pancolitis (Figure 1A and 1B), consistent with ulcerative colitis (UC). He was discharged with a prednisone taper and was started on Vedolizumab. As steroids were tapered, he developed worsening bloody diarrhea, anemia (hemoglobin 2 g/dL), and new thrombocytopenia. He was again admitted to the hospital and found to have autoimmune hemolytic anemia (AIHA) and immune thrombocytopenia (ITP), and he was diagnosed with concurrent Evan’s Syndrome (Table 1). His therapy for UC was changed to infliximab and azathioprine. His Evan’s Syndrome was treated with high dose prednisone 1mg/kg and intravenous immunoglobulin (IVIG). He has responded well to therapy.
Discussion: Evan’s syndrome, often seen with other autoimmune conditions, is the occurrence of two or more immune cytopenias.It commonly includes autoimmune hemolytic anemia (AIHA) and immune thrombocytopenia (ITP), both of which were seen in our patient. Pathogenesis is thought to be related to impaired colonic wall permeability which leads to reabsorption of damaged erythrocytes and red blood cell antigens. Evan’s syndrome in UC often correlates with disease activity, is more likely seen in pan-colonic disease, and is most often diagnosed in the setting of an acute flare, as seen in our patient. While Evan’s Syndrome is a rare EIM, the incidence of autoimmune anemias is significantly higher in patients with IBD (125 per 100,000) than in the general population (18 per 100,000). In caring for patients with IBD, it is important to consider immune cytopenias in patients who have persistent, unexplained anemia or thrombocytopenia.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Erica Graff, MD1, Jenny Jan, MD2, Jeffry Katz, MD3, Vu Q. Nguyen, MD, MS3. P4451 - Evan’s Syndrome in a Patient With Ulcerative Colitis: A Rare Extraintestinal Manifestation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2University Hospitals Cleveland Medical Center, Cleveland, OH; 3Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: Inflammatory bowel disease (IBD) is an autoimmune condition affecting the gastrointestinal tract that can also affect other organ systems. Over 50% of patients with IBD develop extraintestinal manifestations (EIMs), with hematologic EIMs being less common. We present a rare case of a patient with ulcerative colitis and concurrent Evan’s syndrome.
Case Description/Methods: A 44 year-old previously healthy man presented to gastroenterology clinic with more than ten loose, bloody and watery stools daily for the last 2 months. He also had bloating, tenesmus and a 10-pound weight loss over six months. He was pale on physical exam, with labs notable for a hemoglobin of 5 g/dL. He was admitted to the hospital for expedited work-up where colonoscopy showed Mayo 3 pancolitis (Figure 1A and 1B), consistent with ulcerative colitis (UC). He was discharged with a prednisone taper and was started on Vedolizumab. As steroids were tapered, he developed worsening bloody diarrhea, anemia (hemoglobin 2 g/dL), and new thrombocytopenia. He was again admitted to the hospital and found to have autoimmune hemolytic anemia (AIHA) and immune thrombocytopenia (ITP), and he was diagnosed with concurrent Evan’s Syndrome (Table 1). His therapy for UC was changed to infliximab and azathioprine. His Evan’s Syndrome was treated with high dose prednisone 1mg/kg and intravenous immunoglobulin (IVIG). He has responded well to therapy.
Discussion: Evan’s syndrome, often seen with other autoimmune conditions, is the occurrence of two or more immune cytopenias.It commonly includes autoimmune hemolytic anemia (AIHA) and immune thrombocytopenia (ITP), both of which were seen in our patient. Pathogenesis is thought to be related to impaired colonic wall permeability which leads to reabsorption of damaged erythrocytes and red blood cell antigens. Evan’s syndrome in UC often correlates with disease activity, is more likely seen in pan-colonic disease, and is most often diagnosed in the setting of an acute flare, as seen in our patient. While Evan’s Syndrome is a rare EIM, the incidence of autoimmune anemias is significantly higher in patients with IBD (125 per 100,000) than in the general population (18 per 100,000). In caring for patients with IBD, it is important to consider immune cytopenias in patients who have persistent, unexplained anemia or thrombocytopenia.
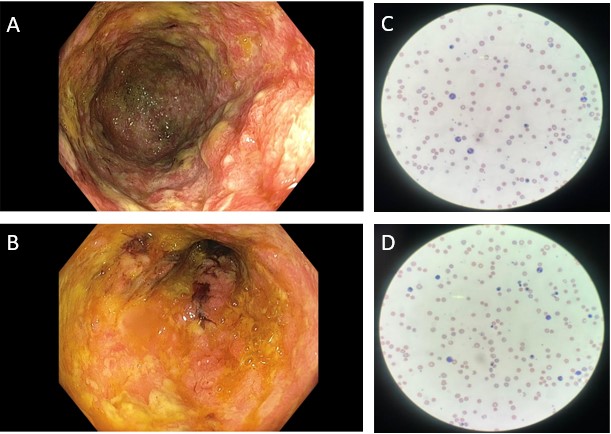
Figure: Mayo 3 Ulcerative pancolitis (A and B) and peripheral smear with marked anemia and an increase in polychromasia and increased nucleated erythroid precursor (C and D).
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Erica Graff indicated no relevant financial relationships.
Jenny Jan indicated no relevant financial relationships.
Jeffry Katz indicated no relevant financial relationships.
Vu Nguyen: AbbVie – Speakers Bureau. Eli Lilly – Speakers Bureau.
Erica Graff, MD1, Jenny Jan, MD2, Jeffry Katz, MD3, Vu Q. Nguyen, MD, MS3. P4451 - Evan’s Syndrome in a Patient With Ulcerative Colitis: A Rare Extraintestinal Manifestation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
