Tuesday Poster Session
Category: Interventional Endoscopy
P4457 - The Impact and Utilization of Magnetic Resonance Cholangiopancreatography (MRCP) Amongst Patients Undergoing Endoscopic Retrograde Cholangiopancreatography (ERCP) in a Community Hospital System
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- RP
Rahul Patel, DO
Jefferson Health
Washington Township, NJ
Presenting Author(s)
Rahul Patel, DO1, Hiral Amin, DO1, Tirth Patel, PhD2, Sachin Prasad, DO1, Kristine Wong, DO1, Shashank Gupta, DO1, Marisa Pope, DO1, C. Jonathan Foster, DO3
1Jefferson Health, Washington Township, NJ; 2Rowan-Virtua School of Osteopathic Medicine, Stratford, NJ; 3Jefferson Health, Cherry Hill, NJ
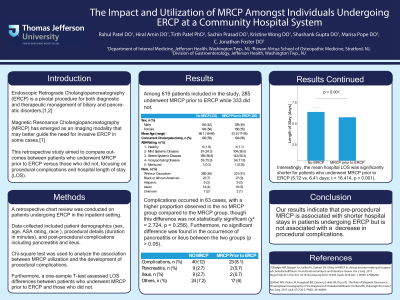
Introduction: ERCP is a pivotal procedure for both diagnostic and therapeutic management of biliary and pancreatic disorders. MRCP has emerged as an alternative imaging modality that may obviate the need for invasive ERCP in some cases. This retrospective study aims to compare outcomes between patients who underwent MRCP prior to ERCP versus those who did not, focusing on procedural complications and hospital length of stay (LOS).
Methods: A retrospective chart review was conducted on patients undergoing ERCP in the inpatient population from a 3 center community hospital. Data collected included patient demographics (age, race, ethnicity, gender), procedural details (duration in minutes), and post-procedural complications including pancreatitis and ileus. Chi-square test was used to analyze the association between MRCP utilization and the development of procedural complications. Furthermore, a T-test assessed LOS differences between patients who underwent MRCP prior to ERCP and those who did not.
Results: Among 619 patients included in the study, 285 underwent MRCP prior to ERCP while 333 did not. Complications occurred in 63 cases, with a higher proportion observed in patients who did not undergo MRCP (63.5%) compared to those who did (36.5%), though this difference was not statistically significant (χ² = 2.724, p = 0.256). Furthermore, no significant difference was found in the occurrence of pancreatitis or ileus between the two groups (p > 0.05). Interestingly, the mean hospital LOS was significantly shorter for patients who underwent MRCP (5.72 days vs. 6.41 days in no MRCP group; t = 16.414, p < 0.001) prior to ERCP.
Discussion: While MRCP has emerged as a valuable minimally invasive diagnostic tool, its utility in improving healthcare outcomes remains uncertain. This study compared post-procedural complications and hospital stay length between patients who underwent MRCP before ERCP and those who did not. Our results indicate that pre-procedural MRCP may contribute to shorter hospital stays in patients undergoing ERCP without increasing the risk of procedural complications. These findings suggest that MRCP may be useful to triage patients for ERCP, potentially optimizing resource allocation and patient outcomes. Further studies are needed to analyze these findings in tertiary care.
Disclosures:
Rahul Patel, DO1, Hiral Amin, DO1, Tirth Patel, PhD2, Sachin Prasad, DO1, Kristine Wong, DO1, Shashank Gupta, DO1, Marisa Pope, DO1, C. Jonathan Foster, DO3. P4457 - The Impact and Utilization of Magnetic Resonance Cholangiopancreatography (MRCP) Amongst Patients Undergoing Endoscopic Retrograde Cholangiopancreatography (ERCP) in a Community Hospital System, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Jefferson Health, Washington Township, NJ; 2Rowan-Virtua School of Osteopathic Medicine, Stratford, NJ; 3Jefferson Health, Cherry Hill, NJ
Introduction: ERCP is a pivotal procedure for both diagnostic and therapeutic management of biliary and pancreatic disorders. MRCP has emerged as an alternative imaging modality that may obviate the need for invasive ERCP in some cases. This retrospective study aims to compare outcomes between patients who underwent MRCP prior to ERCP versus those who did not, focusing on procedural complications and hospital length of stay (LOS).
Methods: A retrospective chart review was conducted on patients undergoing ERCP in the inpatient population from a 3 center community hospital. Data collected included patient demographics (age, race, ethnicity, gender), procedural details (duration in minutes), and post-procedural complications including pancreatitis and ileus. Chi-square test was used to analyze the association between MRCP utilization and the development of procedural complications. Furthermore, a T-test assessed LOS differences between patients who underwent MRCP prior to ERCP and those who did not.
Results: Among 619 patients included in the study, 285 underwent MRCP prior to ERCP while 333 did not. Complications occurred in 63 cases, with a higher proportion observed in patients who did not undergo MRCP (63.5%) compared to those who did (36.5%), though this difference was not statistically significant (χ² = 2.724, p = 0.256). Furthermore, no significant difference was found in the occurrence of pancreatitis or ileus between the two groups (p > 0.05). Interestingly, the mean hospital LOS was significantly shorter for patients who underwent MRCP (5.72 days vs. 6.41 days in no MRCP group; t = 16.414, p < 0.001) prior to ERCP.
Discussion: While MRCP has emerged as a valuable minimally invasive diagnostic tool, its utility in improving healthcare outcomes remains uncertain. This study compared post-procedural complications and hospital stay length between patients who underwent MRCP before ERCP and those who did not. Our results indicate that pre-procedural MRCP may contribute to shorter hospital stays in patients undergoing ERCP without increasing the risk of procedural complications. These findings suggest that MRCP may be useful to triage patients for ERCP, potentially optimizing resource allocation and patient outcomes. Further studies are needed to analyze these findings in tertiary care.
Disclosures:
Rahul Patel indicated no relevant financial relationships.
Hiral Amin indicated no relevant financial relationships.
Tirth Patel indicated no relevant financial relationships.
Sachin Prasad indicated no relevant financial relationships.
Kristine Wong indicated no relevant financial relationships.
Shashank Gupta indicated no relevant financial relationships.
Marisa Pope indicated no relevant financial relationships.
C. Jonathan Foster: Conmed – Consultant. Steris – Consultant.
Rahul Patel, DO1, Hiral Amin, DO1, Tirth Patel, PhD2, Sachin Prasad, DO1, Kristine Wong, DO1, Shashank Gupta, DO1, Marisa Pope, DO1, C. Jonathan Foster, DO3. P4457 - The Impact and Utilization of Magnetic Resonance Cholangiopancreatography (MRCP) Amongst Patients Undergoing Endoscopic Retrograde Cholangiopancreatography (ERCP) in a Community Hospital System, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
