Tuesday Poster Session
Category: Interventional Endoscopy
P4464 - Post-ERCP Cholecystitis Following Covered Self-Expandable Metal Stent Placement in Patients With Malignant Biliary Obstruction: A Meta-Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Chawin Lopimpisuth, MD
University of Miami Miller School of Medicine
Miami, FL
Presenting Author(s)
Chawin Lopimpisuth, MD1, Shyam Vedantam, DO1, Pojsakorn Danpanichkul, MD2, Shria Kumar, MD, MSCE1, Jodie A. Barkin, MD, FACG3, Sunil Amin, MD, MPH1, Sean Bhalla, MD1
1University of Miami Miller School of Medicine, Miami, FL; 2Texas Tech University Health Sciences Center, Lubbock, TX; 3University of Miami Miller School of Medicine, Boca Raton, FL
Introduction: Incidence of postprocedural cholecystitis after endoscopic retrograde cholangiopancreatography (ERCP) for biliary drainage using a covered self-expandable metal stent (CSEMS) for distal malignant biliary obstruction (MBO) has been reported gradually in the past decade. Despite requiring invasive intervention, the complication tends to receive less attention compared to pancreatitis. Moreover, cholecystitis could lead to delay in the patient’s oncologic treatments. Previous studies and meta-analyses have showed conflicting results. We sought to compare acute cholecystitis rates after placement of uncovered self-expandable metal stent (USEMS) versus CSEMS for MBO.
Methods: All clinical studies published up to April 2024 comparing acute cholecystitis rates after USEMS and CSEMS placement for biliary drainage in MBO were identified using electronic bibliographic searches of PubMed, SCOPUS, and The Cochrane Library. The primary outcome was rates of adverse events (AEs). The event rates were pooled using a fixed-effect model. Heterogeneity and publication bias were explored using Egger’s test and funnel plot.
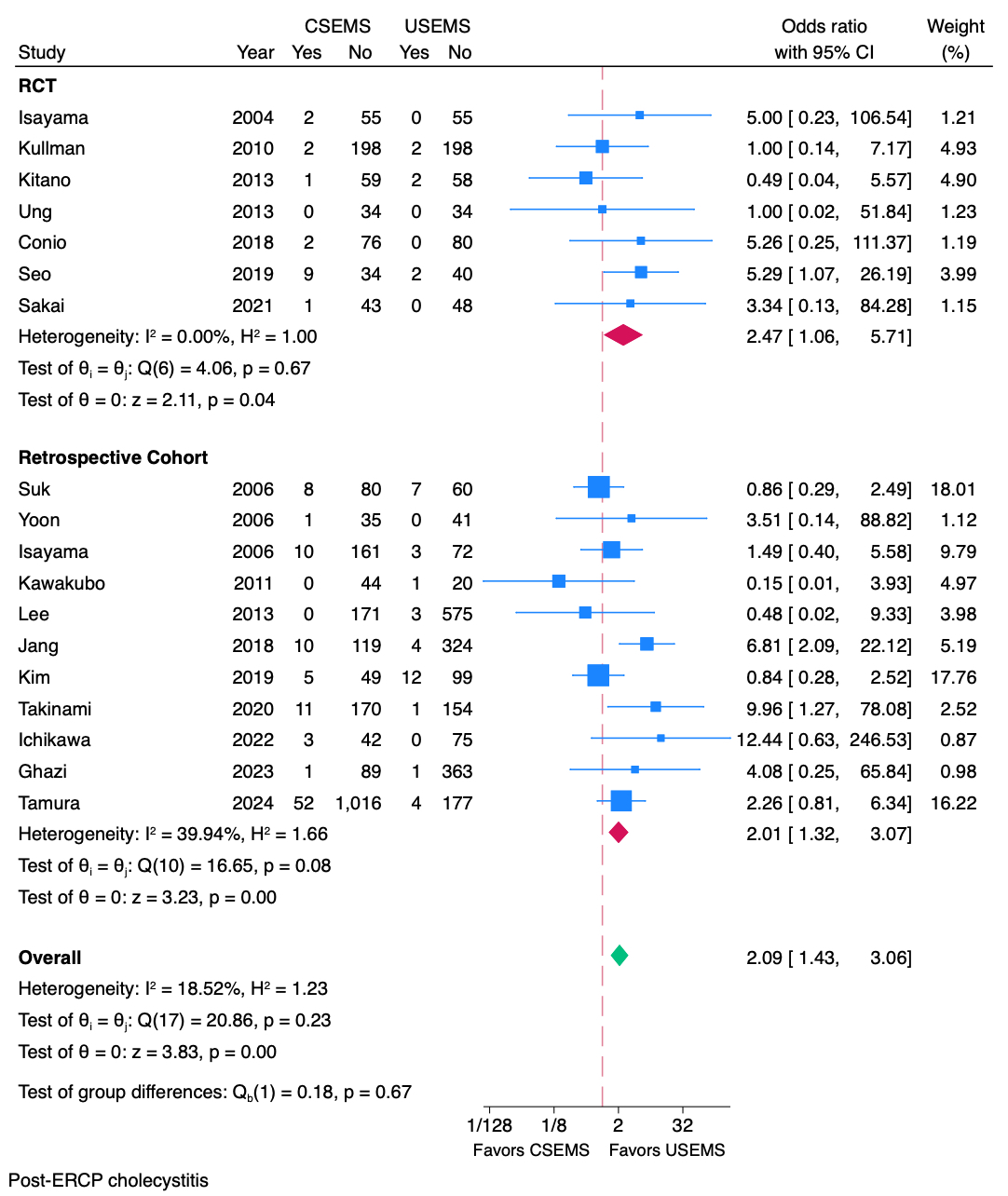
Results: Of 569 articles identified, 18 studies (7 randomized controlled trials (RCTs) vs 11 observational studies) met inclusion criteria for final analysis (2,593 using CSEMS and 2,515 using USEMS). Pooled estimates of CSEMS showed higher post-ERCP acute cholecystitis rates (OR 2.09, 95% confidence interval (CI) 1.43 - 3.06, p < 0.01) (Figure 1), higher acute pancreatitis rates (OR 1.49, 95% CI 1.11 - 2.01, p = 0.01), lower tumor ingrowth rates (OR 0.05, 95% CI 0.03 - 0.08, p < 0.01) and higher rates of stent migration (OR 4.82, 95% CI 2.82 - 8.23, p < 0.01). There was no publication bias detected from funnel plot and Egger’s test (p = 0.82). Subgroup analysis, stratified by type of study, and sensitivity analysis by omitting studies one at a time were performed, and revealed no changes in direction or magnitude of the estimates.
Discussion: Our study findings suggest that CSEMS can lead to higher rates of post-ERCP cholecystitis compared to USEMS. Additionally, subgroup analysis of RCTs showed similar results. Interestingly, the rates of acute pancreatitis were significantly higher in those with CSEMS. Placement of CSEMS for distal MBO carries increased risk of acute cholecystitis compared to USEMS, which should be considered during stent selection to prevent morbidity and delays in treatment.
Disclosures:
Chawin Lopimpisuth, MD1, Shyam Vedantam, DO1, Pojsakorn Danpanichkul, MD2, Shria Kumar, MD, MSCE1, Jodie A. Barkin, MD, FACG3, Sunil Amin, MD, MPH1, Sean Bhalla, MD1. P4464 - Post-ERCP Cholecystitis Following Covered Self-Expandable Metal Stent Placement in Patients With Malignant Biliary Obstruction: A Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Miami Miller School of Medicine, Miami, FL; 2Texas Tech University Health Sciences Center, Lubbock, TX; 3University of Miami Miller School of Medicine, Boca Raton, FL
Introduction: Incidence of postprocedural cholecystitis after endoscopic retrograde cholangiopancreatography (ERCP) for biliary drainage using a covered self-expandable metal stent (CSEMS) for distal malignant biliary obstruction (MBO) has been reported gradually in the past decade. Despite requiring invasive intervention, the complication tends to receive less attention compared to pancreatitis. Moreover, cholecystitis could lead to delay in the patient’s oncologic treatments. Previous studies and meta-analyses have showed conflicting results. We sought to compare acute cholecystitis rates after placement of uncovered self-expandable metal stent (USEMS) versus CSEMS for MBO.
Methods: All clinical studies published up to April 2024 comparing acute cholecystitis rates after USEMS and CSEMS placement for biliary drainage in MBO were identified using electronic bibliographic searches of PubMed, SCOPUS, and The Cochrane Library. The primary outcome was rates of adverse events (AEs). The event rates were pooled using a fixed-effect model. Heterogeneity and publication bias were explored using Egger’s test and funnel plot.
Results: Of 569 articles identified, 18 studies (7 randomized controlled trials (RCTs) vs 11 observational studies) met inclusion criteria for final analysis (2,593 using CSEMS and 2,515 using USEMS). Pooled estimates of CSEMS showed higher post-ERCP acute cholecystitis rates (OR 2.09, 95% confidence interval (CI) 1.43 - 3.06, p < 0.01) (Figure 1), higher acute pancreatitis rates (OR 1.49, 95% CI 1.11 - 2.01, p = 0.01), lower tumor ingrowth rates (OR 0.05, 95% CI 0.03 - 0.08, p < 0.01) and higher rates of stent migration (OR 4.82, 95% CI 2.82 - 8.23, p < 0.01). There was no publication bias detected from funnel plot and Egger’s test (p = 0.82). Subgroup analysis, stratified by type of study, and sensitivity analysis by omitting studies one at a time were performed, and revealed no changes in direction or magnitude of the estimates.
Discussion: Our study findings suggest that CSEMS can lead to higher rates of post-ERCP cholecystitis compared to USEMS. Additionally, subgroup analysis of RCTs showed similar results. Interestingly, the rates of acute pancreatitis were significantly higher in those with CSEMS. Placement of CSEMS for distal MBO carries increased risk of acute cholecystitis compared to USEMS, which should be considered during stent selection to prevent morbidity and delays in treatment.
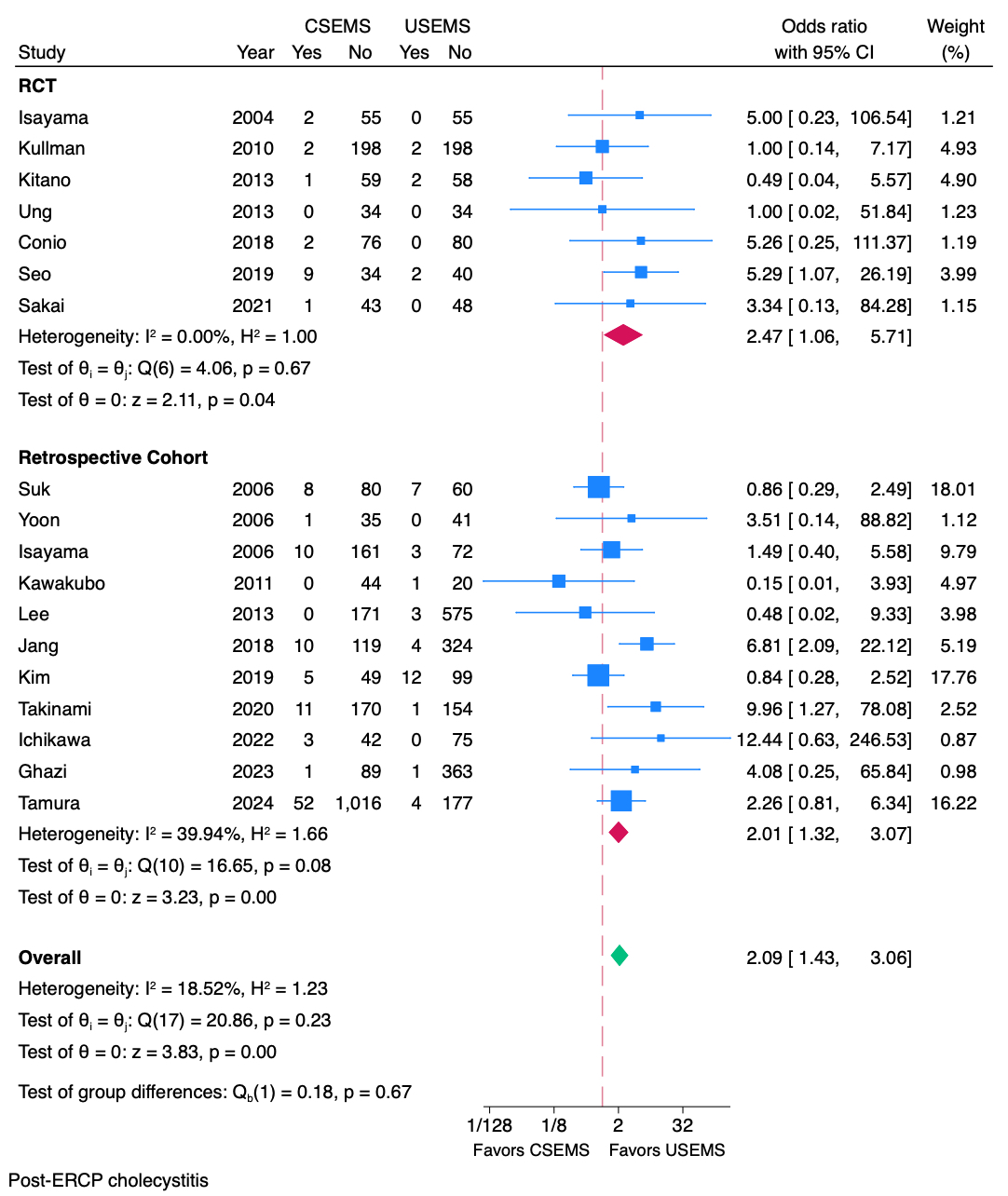
Figure: Figure 1 – Pooled estimate of post-ERCP cholecystitis following covered vs uncovered metal stent placement
Disclosures:
Chawin Lopimpisuth indicated no relevant financial relationships.
Shyam Vedantam indicated no relevant financial relationships.
Pojsakorn Danpanichkul indicated no relevant financial relationships.
Shria Kumar indicated no relevant financial relationships.
Jodie Barkin: Abbvie – Consultant. Aimmune Therapeutics – Consultant. Corevitas – Consultant. Exact Sciences – Consultant. Medtronic – Consultant. Motus GI – Consultant. Organon – Consultant.
Sunil Amin: 3D Matrix – Consultant. Boston Scientific – Consultant. Medtronic – Consultant.
Sean Bhalla indicated no relevant financial relationships.
Chawin Lopimpisuth, MD1, Shyam Vedantam, DO1, Pojsakorn Danpanichkul, MD2, Shria Kumar, MD, MSCE1, Jodie A. Barkin, MD, FACG3, Sunil Amin, MD, MPH1, Sean Bhalla, MD1. P4464 - Post-ERCP Cholecystitis Following Covered Self-Expandable Metal Stent Placement in Patients With Malignant Biliary Obstruction: A Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
