Tuesday Poster Session
Category: Interventional Endoscopy
P4485 - Determinants of Endoscopic Ultrasound Utilization and Survival Outcomes in Gastric Adenocarcinoma: Insights from SEER
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- CB
Christopher A. Bouvette, MD
University of Oklahoma College of Medicine
Oklahoma City, OK
Presenting Author(s)
Christopher A. Bouvette, MD1, Gledius Kola, MS2, Alyssa Grossen, MD1, Ryan Nipp, MD, MPH1, Kai Ding, PhD3, Amir Rumman, MD1
1University of Oklahoma College of Medicine, Oklahoma City, OK; 2University of Oklahoma Health Sciences Center, Oklahoma City, OK; 3Oklahoma University Health Sciences Center, Oklahoma City, OK
Introduction: Endoscopic ultrasound (EUS) is widely established in the diagnosis and staging of gastric malignancy. It excels in establishing depth of gastric wall involvement and evaluation of peri-gastric lymph nodes. We hypothesized sociodemographic determinants may predict receipt of EUS, and ultimately that staging EUS would be associated with survival outcomes.
Methods: We conducted a retrospective cohort study of the SEER dataset linked with Medicare claims for gastric cancer. The cohort was limited to gastric adenocarcinoma (GAC). The base file assessed receipt of chemotherapy, radiation, or surgery. We then determined receipt of EUS and type of surgery (partial or total gastrectomy) through associated claims. We used multivariable logistic regression to identify factors associated with receipt of EUS. We used Kaplan-Meier estimates and Cox regression modeling to explore associations of EUS with stage-specific survival.
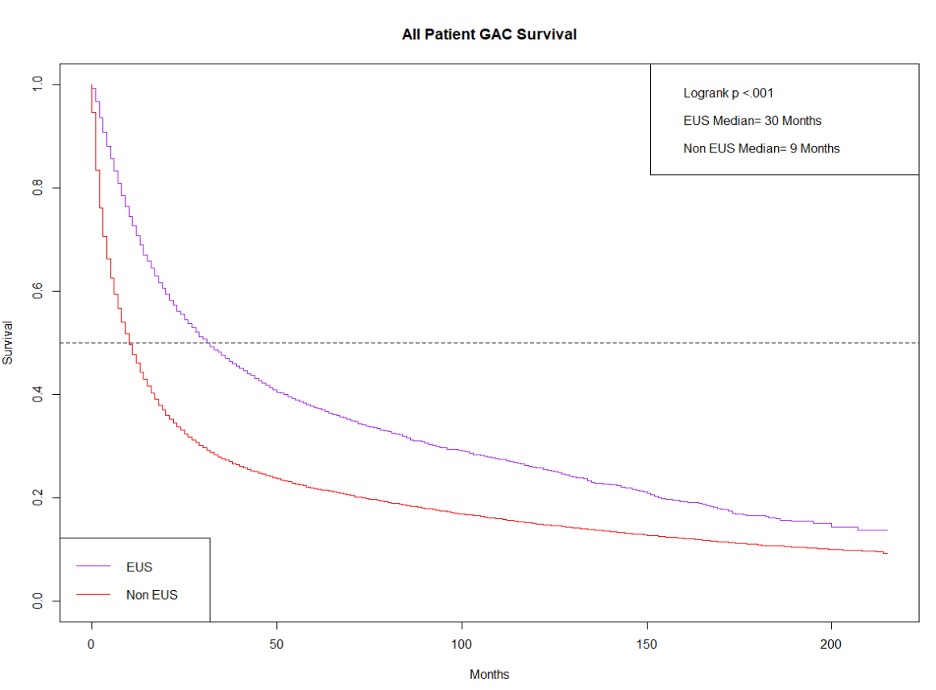
Results: Overall, 59,914 patients with GAC were included in this analysis. Only 14% of patients received EUS. Factors significantly (p< 0.0001) associated with decreased likelihood of receiving EUS included: age 80 or older (OR 0.85), black race (OR 0.54), lower income (OR 0.86), lower education (OR 0.76), regional (0.63) or distant stage (OR 0.28), localizing to the lesser/greater curvature (OR 0.73) or overlapping (OR 0.72), and not receiving chemotherapy (OR 0.62) or radiation (0.61). Factors significantly (p< 0.0001) associated with increased likelihood of receiving EUS included: being married (OR 1.15), residence in the Midwest (OR 1.84), Northeast (OR 1.96), or West Coast (OR 1.30), Charlson Comorbidity Index 2 or greater (OR 1.35), and receipt of partial (OR 1.23) or total gastrectomy (OR 1.79). Patients who received EUS had a significantly higher median survival (30 vs 9 months, logrank p< 0.001, Figure 1). When excluding patients with distant disease, Cox regression modeling demonstrated lower mortality risk associated with receipt EUS (HR 0.75, p< 0.0001).
Discussion: Receipt of EUS locoregional staging was associated with a lower mortality risk. EUS remains under-utilized, with only 14% utilization across this nationwide sample. Clinical (age greater than 80, regional or distant stage disease, origination at the lesser/greater curvature) and non-clinical factors (black race, lower education, and lower income) negatively predict receipt of staging EUS. Collectively, these results highlight the utility of EUS in GAC while underscoring disparities in care delivery.
Disclosures:
Christopher A. Bouvette, MD1, Gledius Kola, MS2, Alyssa Grossen, MD1, Ryan Nipp, MD, MPH1, Kai Ding, PhD3, Amir Rumman, MD1. P4485 - Determinants of Endoscopic Ultrasound Utilization and Survival Outcomes in Gastric Adenocarcinoma: Insights from SEER, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Oklahoma College of Medicine, Oklahoma City, OK; 2University of Oklahoma Health Sciences Center, Oklahoma City, OK; 3Oklahoma University Health Sciences Center, Oklahoma City, OK
Introduction: Endoscopic ultrasound (EUS) is widely established in the diagnosis and staging of gastric malignancy. It excels in establishing depth of gastric wall involvement and evaluation of peri-gastric lymph nodes. We hypothesized sociodemographic determinants may predict receipt of EUS, and ultimately that staging EUS would be associated with survival outcomes.
Methods: We conducted a retrospective cohort study of the SEER dataset linked with Medicare claims for gastric cancer. The cohort was limited to gastric adenocarcinoma (GAC). The base file assessed receipt of chemotherapy, radiation, or surgery. We then determined receipt of EUS and type of surgery (partial or total gastrectomy) through associated claims. We used multivariable logistic regression to identify factors associated with receipt of EUS. We used Kaplan-Meier estimates and Cox regression modeling to explore associations of EUS with stage-specific survival.
Results: Overall, 59,914 patients with GAC were included in this analysis. Only 14% of patients received EUS. Factors significantly (p< 0.0001) associated with decreased likelihood of receiving EUS included: age 80 or older (OR 0.85), black race (OR 0.54), lower income (OR 0.86), lower education (OR 0.76), regional (0.63) or distant stage (OR 0.28), localizing to the lesser/greater curvature (OR 0.73) or overlapping (OR 0.72), and not receiving chemotherapy (OR 0.62) or radiation (0.61). Factors significantly (p< 0.0001) associated with increased likelihood of receiving EUS included: being married (OR 1.15), residence in the Midwest (OR 1.84), Northeast (OR 1.96), or West Coast (OR 1.30), Charlson Comorbidity Index 2 or greater (OR 1.35), and receipt of partial (OR 1.23) or total gastrectomy (OR 1.79). Patients who received EUS had a significantly higher median survival (30 vs 9 months, logrank p< 0.001, Figure 1). When excluding patients with distant disease, Cox regression modeling demonstrated lower mortality risk associated with receipt EUS (HR 0.75, p< 0.0001).
Discussion: Receipt of EUS locoregional staging was associated with a lower mortality risk. EUS remains under-utilized, with only 14% utilization across this nationwide sample. Clinical (age greater than 80, regional or distant stage disease, origination at the lesser/greater curvature) and non-clinical factors (black race, lower education, and lower income) negatively predict receipt of staging EUS. Collectively, these results highlight the utility of EUS in GAC while underscoring disparities in care delivery.
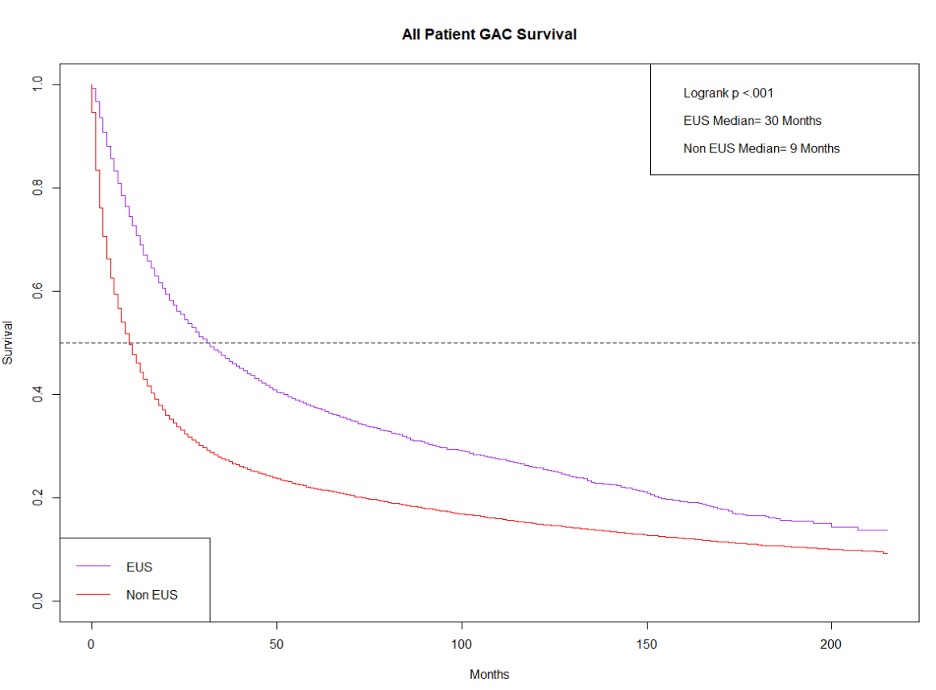
Figure: Figure 1
Disclosures:
Christopher Bouvette indicated no relevant financial relationships.
Gledius Kola indicated no relevant financial relationships.
Alyssa Grossen indicated no relevant financial relationships.
Ryan Nipp indicated no relevant financial relationships.
Kai Ding indicated no relevant financial relationships.
Amir Rumman indicated no relevant financial relationships.
Christopher A. Bouvette, MD1, Gledius Kola, MS2, Alyssa Grossen, MD1, Ryan Nipp, MD, MPH1, Kai Ding, PhD3, Amir Rumman, MD1. P4485 - Determinants of Endoscopic Ultrasound Utilization and Survival Outcomes in Gastric Adenocarcinoma: Insights from SEER, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

