Tuesday Poster Session
Category: Interventional Endoscopy
P4489 - Analysis of Reported Adverse Events Related to The Use of Radio-Frequency Ablation (RFA) Catheters: An FDA MAUDE Database Study
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ayman Elawad, MD
Massachusetts General Hospital
Boston, MA
Presenting Author(s)
Ayman Elawad, MD1, Elmkdad E. Mohammed, MD2, Shaikhoon Mohammed, MD3, Mohanad Awadalla, MD4, Abdellatif Ismail, MD5, Natalie Wilson, MD6, Khalid Ahmed, MD7, Marwa Salman, MBBS8, Mohamed Abdallah, MD9, Prabhleen Chahal, MD10, Mohammad Bilal, MD11
1Massachusetts General Hospital, Boston, MA; 2The Wright Center for Graduate Medical Education, Scranton, PA; 3Macon Medical Group PC, Atlanta, GA; 4Beth Israel Deaconess Medical Center, Boston, MA; 5University of Maryland Medical Center, Baltimore, MD; 6University of Minnesota, Minneapolis, MN; 7University of Pennsylvania, Philadelphia, PA; 8University of Medical Sciences and Technology, Khartoum, Sudan, Philadelphia, PA; 9Cleveland Clinic, Cleveland, OH; 10Cleveland Clinic Foundation, Cleveland, OH; 11University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Biliary radiofrequency ablation (RFA) catheters can ablate pre-cancerous and cancerous pancreatic or biliary tract tissue. Habib™ EndoHPB Catheter was approved by the FDA in 2009 for pancreatic and biliary tumor palliation. However, little is known about the adverse events (AEs) associated with the use of biliary RFA catheters. We aimed to analyze AEs associated with the biliary RFA catheter using the Food and Drug Administration (FDA)"Manufacturer and User Facility Device Experience" (MAUDE) database.
Methods: We analyzed the post-marketing surveillance data from the FDA’s MAUDE database for the biliary RFA catheter from January 2014 through May 2024. The search results were classified into patient-related AEs and device-related technical issues.
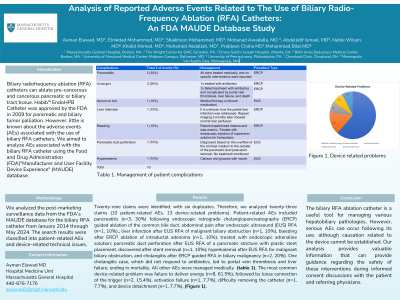
Results: Twenty-nine claims were identified, with six duplicates. Therefore, we analyzed twenty-three claims (10 patient-related AEs, 13 device-related problems). Patient-related AEs included pancreatitis (n=3, 30%) following endoscopic retrograde cholangiopancreatography (ERCP) guided ablation of the common bile duct, abdominal pain after endoscopic ultrasound (EUS) RFA (n=1, 10%),; liver infarction after EUS RFA of malignant biliary obstruction (n=1, 10%), bleeding after ERCP ablation of intraductal adenoma (n=1, 10%), treated with endoscopic adrenaline solution; pancreatic duct perforation after EUS RFA of a pancreatic stricture with plastic stent placement, discovered after stent removal (n=1, 10%); hyperkalemia after EUS RFA for malignant biliary obstruction, and cholangitis after ERCP guided RFA in biliary malignancy (n=2, 20%). One cholangitis case, which did not respond to antibiotics, led to portal vein thrombosis and liver failure, ending in mortality. All other AEs were managed medically (table 1). The most common device-related problem was failure to deliver energy (n=8, 61.5%), followed by loose connection of the trigger (n=2, 15.4%), activation failure (n=1, 7.7%), difficulty removing the catheter (n=1, 7.7%), and device detachment (n=1, 7.7%), (Figure 1).
Discussion: The biliary RFA ablation catheter is a useful tool for managing various hepatobiliary pathologies. However, serious AEs can occur following its use, although causation related to the device cannot be established. Our analysis provides valuable information that can provide guidance regarding the safety of these interventions during informed consent discussions with the patient and referring physicians.

Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ayman Elawad, MD1, Elmkdad E. Mohammed, MD2, Shaikhoon Mohammed, MD3, Mohanad Awadalla, MD4, Abdellatif Ismail, MD5, Natalie Wilson, MD6, Khalid Ahmed, MD7, Marwa Salman, MBBS8, Mohamed Abdallah, MD9, Prabhleen Chahal, MD10, Mohammad Bilal, MD11. P4489 - Analysis of Reported Adverse Events Related to The Use of Radio-Frequency Ablation (RFA) Catheters: An FDA MAUDE Database Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Massachusetts General Hospital, Boston, MA; 2The Wright Center for Graduate Medical Education, Scranton, PA; 3Macon Medical Group PC, Atlanta, GA; 4Beth Israel Deaconess Medical Center, Boston, MA; 5University of Maryland Medical Center, Baltimore, MD; 6University of Minnesota, Minneapolis, MN; 7University of Pennsylvania, Philadelphia, PA; 8University of Medical Sciences and Technology, Khartoum, Sudan, Philadelphia, PA; 9Cleveland Clinic, Cleveland, OH; 10Cleveland Clinic Foundation, Cleveland, OH; 11University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Biliary radiofrequency ablation (RFA) catheters can ablate pre-cancerous and cancerous pancreatic or biliary tract tissue. Habib™ EndoHPB Catheter was approved by the FDA in 2009 for pancreatic and biliary tumor palliation. However, little is known about the adverse events (AEs) associated with the use of biliary RFA catheters. We aimed to analyze AEs associated with the biliary RFA catheter using the Food and Drug Administration (FDA)"Manufacturer and User Facility Device Experience" (MAUDE) database.
Methods: We analyzed the post-marketing surveillance data from the FDA’s MAUDE database for the biliary RFA catheter from January 2014 through May 2024. The search results were classified into patient-related AEs and device-related technical issues.
Results: Twenty-nine claims were identified, with six duplicates. Therefore, we analyzed twenty-three claims (10 patient-related AEs, 13 device-related problems). Patient-related AEs included pancreatitis (n=3, 30%) following endoscopic retrograde cholangiopancreatography (ERCP) guided ablation of the common bile duct, abdominal pain after endoscopic ultrasound (EUS) RFA (n=1, 10%),; liver infarction after EUS RFA of malignant biliary obstruction (n=1, 10%), bleeding after ERCP ablation of intraductal adenoma (n=1, 10%), treated with endoscopic adrenaline solution; pancreatic duct perforation after EUS RFA of a pancreatic stricture with plastic stent placement, discovered after stent removal (n=1, 10%); hyperkalemia after EUS RFA for malignant biliary obstruction, and cholangitis after ERCP guided RFA in biliary malignancy (n=2, 20%). One cholangitis case, which did not respond to antibiotics, led to portal vein thrombosis and liver failure, ending in mortality. All other AEs were managed medically (table 1). The most common device-related problem was failure to deliver energy (n=8, 61.5%), followed by loose connection of the trigger (n=2, 15.4%), activation failure (n=1, 7.7%), difficulty removing the catheter (n=1, 7.7%), and device detachment (n=1, 7.7%), (Figure 1).
Discussion: The biliary RFA ablation catheter is a useful tool for managing various hepatobiliary pathologies. However, serious AEs can occur following its use, although causation related to the device cannot be established. Our analysis provides valuable information that can provide guidance regarding the safety of these interventions during informed consent discussions with the patient and referring physicians.

Figure:
Figure 1. Device related problems
Figure 1. Device related problems
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ayman Elawad indicated no relevant financial relationships.
Elmkdad Mohammed indicated no relevant financial relationships.
Shaikhoon Mohammed indicated no relevant financial relationships.
Mohanad Awadalla indicated no relevant financial relationships.
Abdellatif Ismail indicated no relevant financial relationships.
Natalie Wilson indicated no relevant financial relationships.
Khalid Ahmed indicated no relevant financial relationships.
Marwa Salman indicated no relevant financial relationships.
Mohamed Abdallah indicated no relevant financial relationships.
Prabhleen Chahal: Boston Scientific – Advisor or Review Panel Member.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Speakers Bureau.
Ayman Elawad, MD1, Elmkdad E. Mohammed, MD2, Shaikhoon Mohammed, MD3, Mohanad Awadalla, MD4, Abdellatif Ismail, MD5, Natalie Wilson, MD6, Khalid Ahmed, MD7, Marwa Salman, MBBS8, Mohamed Abdallah, MD9, Prabhleen Chahal, MD10, Mohammad Bilal, MD11. P4489 - Analysis of Reported Adverse Events Related to The Use of Radio-Frequency Ablation (RFA) Catheters: An FDA MAUDE Database Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
