Tuesday Poster Session
Category: Interventional Endoscopy
P4497 - Assessing the Efficacy and Safety of EUS-RFA in Pancreatic Adenocarcinoma: A Systematic Review and Meta-Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- KB
Khyati Bidani, MD
Saint Peter's University Hospital
New Brunswick, NJ
Presenting Author(s)
Khyati Bidani, MD1, Vishali Moond, MD1, Ameya Kasture, 2, Ruchir Damjibhai. Paladiya, MBBS3, Amna Iqbal, MD4, Prateek Harne, MD5, Nirav Thosani, MD5
1Saint Peter's University Hospital, New Brunswick, NJ; 2SBHGMC, Mumbai, Maharashtra, India; 3University of Connecticut Health Center, Hartford, CT; 4University of Toledo Medical Center, Toledo, OH; 5McGovern Medical School at UTHealth, Houston, TX
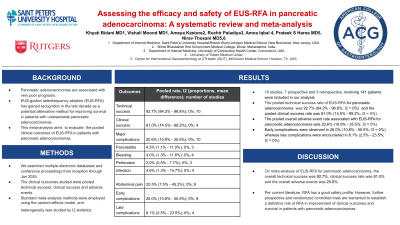
Introduction: Pancreatic adenocarcinomas are associated with very poor prognosis. EUS-guided radiofrequency ablation (EUS-RFA) has gained recognition in the last decade as a potential alternative method for improving survival in patients with unresectable pancreatic adenocarcinomas. However, there is insufficient data regarding the long-term clinical outcomes and overall safety profile of EUS-RFA in such cases. In this meta-analysis, we aim to study the pooled clinical outcomes of EUS-RFA in patients with pancreatic adenocarcinomas.
Methods: We searched multiple electronic databases and conference proceedings from inception through Jan 2024. The clinical outcomes studied were pooled technical success, clinical success and adverse events. Standard meta-analysis methods were employed using the random-effects model, and heterogeneity was studied by I2 statistics.
Results: We analyzed 10 studies, 7 prospective and 3 retrospective, involving 141 patients (42.6% females with a mean age of 63.72 years) having mean tumor size of 41.67 cm and a mean duration follow-up of 14.74 months. Technical success was assessed on a per session basis, and was defined by EUS‐guided access to target lesions along with the completion of the planned ablation procedure. Clinical success was defined as reduction in tumor size or evidence of necrosis on follow up cross-sectional imaging.
The pooled technical success rate of EUS-RFA for pancreatic adenocarcinoma was 92.7% (84.2% - 96.8%; I2 = 0%) and the pooled clinical success rate was 81.0% (14.5% - 99.2%; I2 = 0%). The pooled overall adverse event rate associated with EUS-RFA was 20.6% (10.9% - 35.5%; I2 = 0%). The pooled rates of pancreatitis, bleeding, perforation, infection, and abdominal pain associated per procedure were as follows: 4.3% (1% - 11%; I2 = 0%); 4.0% (1.3% - 11.8%; I2 = 0%); 2.0% (0.5% - 7.7%; I2 = 0%); 4.6% (1.3% - 14.7%; I2 = 0%) and 20.5% (7.5% - 45.2%; I2 = 0%), respectively. Early complications were observed in 26.0% (10.8% - 50.5%; I2 = 0%) whereas late complications were encountered in 8.1% (2.5% - 23.5%; I2 = 0%).
Discussion: On meta-analysis of EUS-RFA for pancreatic adenocarcinoma, the overall technical success was 92.7%, clinical success rate was 81.0% and the overall adverse events was 20.6%. Per current literature, RFA has a good safety profile. However, further prospective and randomized controlled trials are warranted to establish a definitive role of RFA in improvement of clinical outcomes and survival in patients with pancreatic adenocarcinoma.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Khyati Bidani, MD1, Vishali Moond, MD1, Ameya Kasture, 2, Ruchir Damjibhai. Paladiya, MBBS3, Amna Iqbal, MD4, Prateek Harne, MD5, Nirav Thosani, MD5. P4497 - Assessing the Efficacy and Safety of EUS-RFA in Pancreatic Adenocarcinoma: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Saint Peter's University Hospital, New Brunswick, NJ; 2SBHGMC, Mumbai, Maharashtra, India; 3University of Connecticut Health Center, Hartford, CT; 4University of Toledo Medical Center, Toledo, OH; 5McGovern Medical School at UTHealth, Houston, TX
Introduction: Pancreatic adenocarcinomas are associated with very poor prognosis. EUS-guided radiofrequency ablation (EUS-RFA) has gained recognition in the last decade as a potential alternative method for improving survival in patients with unresectable pancreatic adenocarcinomas. However, there is insufficient data regarding the long-term clinical outcomes and overall safety profile of EUS-RFA in such cases. In this meta-analysis, we aim to study the pooled clinical outcomes of EUS-RFA in patients with pancreatic adenocarcinomas.
Methods: We searched multiple electronic databases and conference proceedings from inception through Jan 2024. The clinical outcomes studied were pooled technical success, clinical success and adverse events. Standard meta-analysis methods were employed using the random-effects model, and heterogeneity was studied by I2 statistics.
Results: We analyzed 10 studies, 7 prospective and 3 retrospective, involving 141 patients (42.6% females with a mean age of 63.72 years) having mean tumor size of 41.67 cm and a mean duration follow-up of 14.74 months. Technical success was assessed on a per session basis, and was defined by EUS‐guided access to target lesions along with the completion of the planned ablation procedure. Clinical success was defined as reduction in tumor size or evidence of necrosis on follow up cross-sectional imaging.
The pooled technical success rate of EUS-RFA for pancreatic adenocarcinoma was 92.7% (84.2% - 96.8%; I2 = 0%) and the pooled clinical success rate was 81.0% (14.5% - 99.2%; I2 = 0%). The pooled overall adverse event rate associated with EUS-RFA was 20.6% (10.9% - 35.5%; I2 = 0%). The pooled rates of pancreatitis, bleeding, perforation, infection, and abdominal pain associated per procedure were as follows: 4.3% (1% - 11%; I2 = 0%); 4.0% (1.3% - 11.8%; I2 = 0%); 2.0% (0.5% - 7.7%; I2 = 0%); 4.6% (1.3% - 14.7%; I2 = 0%) and 20.5% (7.5% - 45.2%; I2 = 0%), respectively. Early complications were observed in 26.0% (10.8% - 50.5%; I2 = 0%) whereas late complications were encountered in 8.1% (2.5% - 23.5%; I2 = 0%).
Discussion: On meta-analysis of EUS-RFA for pancreatic adenocarcinoma, the overall technical success was 92.7%, clinical success rate was 81.0% and the overall adverse events was 20.6%. Per current literature, RFA has a good safety profile. However, further prospective and randomized controlled trials are warranted to establish a definitive role of RFA in improvement of clinical outcomes and survival in patients with pancreatic adenocarcinoma.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Khyati Bidani indicated no relevant financial relationships.
Vishali Moond indicated no relevant financial relationships.
Ameya Kasture indicated no relevant financial relationships.
Ruchir Paladiya indicated no relevant financial relationships.
Amna Iqbal indicated no relevant financial relationships.
Prateek Harne indicated no relevant financial relationships.
Nirav Thosani indicated no relevant financial relationships.
Khyati Bidani, MD1, Vishali Moond, MD1, Ameya Kasture, 2, Ruchir Damjibhai. Paladiya, MBBS3, Amna Iqbal, MD4, Prateek Harne, MD5, Nirav Thosani, MD5. P4497 - Assessing the Efficacy and Safety of EUS-RFA in Pancreatic Adenocarcinoma: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
